Governance
Achieving Universal Health Coverage in India
The editorial is based on “The First Step to Universal Healthcare: Make Diagnostics Accessible and Cheap,” published in The Indian Express on 11/08/2025. It emphasizes the critical role of diagnostics in achieving Universal Health Coverage (UHC) in India, focusing on strengthening healthcare infrastructure, digital health initiatives, and capacity building across the country.
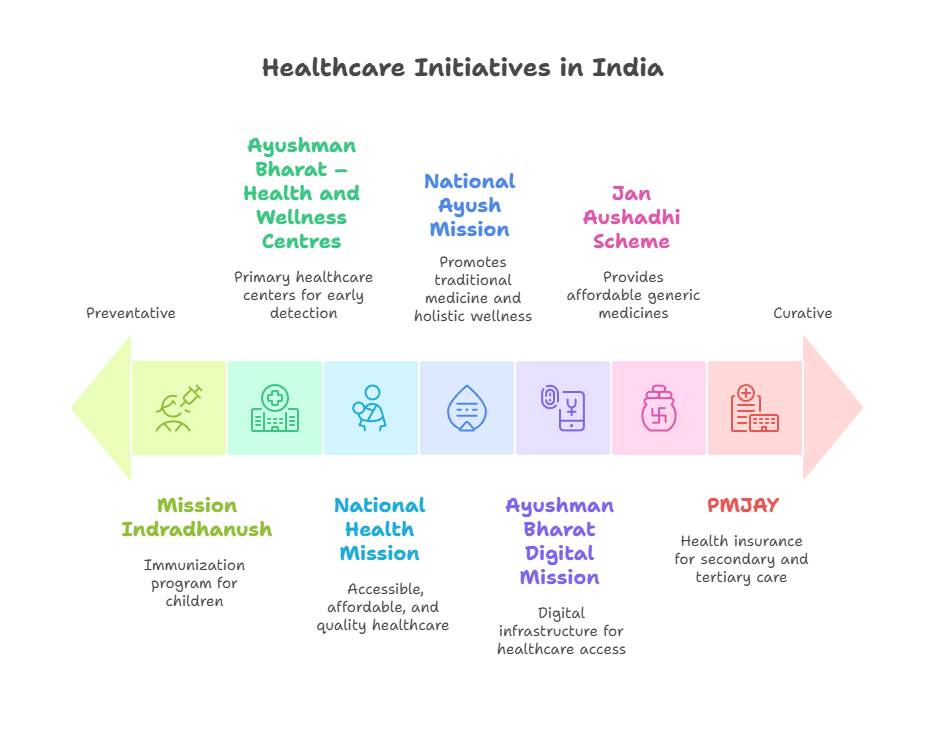
For Prelims: Ayushman Bharat, Ayushman Arogya Mandir, Ayushman Bharat Digital Mission, Non-communicable diseases, Medical Device Policy 2023, PM-Ayushman Bharat Health Infrastructure Mission (2020), Pradhan Mantri Jan Arogya Yojana (PM-JAY)
For Mains: Healthcare sector in India: Related challenges & Way Forward
Universal Health Coverage (UHC) is a fundamental goal of India’s healthcare policy, aiming to provide equitable and affordable healthcare services to all citizens. While significant progress has been made in expanding access, challenges remain, particularly in primary care. Moving forward, India must focus on bridging the existing gaps in healthcare infrastructure, improving service delivery in underserved regions, and ensuring that essential healthcare services are accessible to all, thereby achieving comprehensive healthcare coverage across the country.
What are the Key Developments in India’s Healthcare Sector?
- Expansion of Healthcare Infrastructure: The expansion of government hospitals, medical colleges, and healthcare infrastructure is pivotal in addressing the evolving healthcare needs of India’s rapidly growing population.
- From 2005 to 2021, the number of public hospitals in India surged from 7,008 to 60,621, reflecting a Compound Annual Growth Rate (CAGR) of approximately 14.4%.
- The government’s commitment to expanding health infrastructure is evident through initiatives like the PM-Ayushman Bharat Health Infrastructure Mission (2020).
- From 2018-19 to 2023-24, the Ayushman Aarogya Mandirs (AAMs) have grown at a CAGR of 46.6%, reflecting the increasing commitment to expanding primary healthcare services across India.
- Healthcare Delivery through Digital Innovation: India has embraced the digital health revolution, transforming the healthcare delivery system.
- Initiatives such as the Ayushman Bharat Digital Mission(ABDM), CoWIN App, e-Sanjeevani, and e-Hospital represent a paradigm shift in the country’s healthcare structure.
- The "Scan & Share" service under ABDM, which uses QR codes for faster OPD registration, is gaining traction in hospitals, streamlining patient flow and reducing waiting times.
- By leveraging digital technologies, these efforts make healthcare services accessible to even the most remote areas of the country.
- Initiatives such as the Ayushman Bharat Digital Mission(ABDM), CoWIN App, e-Sanjeevani, and e-Hospital represent a paradigm shift in the country’s healthcare structure.
- Growth in the Pharmaceutical Industry: India ranks third in global pharmaceutical production by volume and is known as the "pharmacy of the world." Its medicines are preferred worldwide due to their low cost and high quality.
- India’s pharmaceutical sector is projected to reach a market size of USD 130 billion by 2030, as per FICCI.
- India also accounts for 60% of global vaccine production making it the largest vaccine producer in the world.
- India’s pharmaceutical sector is projected to reach a market size of USD 130 billion by 2030, as per FICCI.
- Increase in Healthcare Investment: Healthcare financing in India has seen a significant increase in recent years.
- The share of healthcare expenditure as a percentage of GDP has grown from 1.2% in 2014-15 to 2.1% in 2022-23.
- This increase in healthcare funding is crucial for improving the availability and quality of healthcare services nationwide.
- Moreover, India has made significant progress in improving healthcare quality through the establishment of National Quality Standards (NQAS).
- The number of NQAS-certified public health facilities has increased from just 10 in 2016-17 to over 2,000 in 2023-24, reflecting a strong commitment to improving healthcare quality at all levels of service delivery.
- The share of healthcare expenditure as a percentage of GDP has grown from 1.2% in 2014-15 to 2.1% in 2022-23.
- Reduction in Out-of-Pocket Expenditure (OOPE): The shift from the Rashtriya Swasthya Bima Yojana (RSBY) to the Pradhan Mantri Jan Arogya Yojana (PM-JAY), the world’s largest government-funded health assurance scheme, has played a vital role in reducing OOPE.
- PM-JAY extends coverage to nearly 12 crore families, with INR 5 lakh per family annually, encompassing secondary and tertiary care with 1,900 packages and no pre-existing condition exclusions.
- From 64.2% in 2013-14, OOPE has dropped to 47.1% in 2019-20, improving the affordability and accessibility of healthcare services for millions of citizens.
- Strengthening Community Engagement: Initiatives like Jan Arogya Samitis, Mahila Arogya Samitis, and the involvement of Accredited Social Health Activists (ASHAs) have empowered local communities to actively participate in healthcare decision-making and service delivery.
- ASHAs, in particular, play a critical role in bridging the gap between formal healthcare systems and communities.
- The number of ASHA workers has grown by 1.8% CAGR from 8.95 lakh in 2013-14 to 10.65 lakh in 2023-24, indicating the increasing importance of community-driven healthcare.
- ASHAs, in particular, play a critical role in bridging the gap between formal healthcare systems and communities.
What are the Key Barriers to Achieving Universal Health Coverage in India?
- Inadequate Healthcare Infrastructure: Despite the improvements in India's healthcare sector, the country continues to face a significant shortage of healthcare facilities, particularly in rural areas where the majority of the population resides.
- Many PHCs and sub-centers still lack essential infrastructure, medical equipment, and resources, making it challenging to provide even basic healthcare services.
- This shortage further exacerbates the existing difficulties in ensuring the delivery of quality healthcare to rural populations.
- According to the National Health Profile of 2021, India has 0.6 beds per 1,000 people, which is lower than what was recommended in the National Health Policy, 2017.
- Many PHCs and sub-centers still lack essential infrastructure, medical equipment, and resources, making it challenging to provide even basic healthcare services.
- Shortage and Uneven Distribution of Healthcare Professionals: India faces a significant shortage of healthcare professionals which is a critical challenge for the healthcare system, impacting the quality and accessibility of services.
- While WHO recommends 44.5 doctors, nurses, and midwives per 10,000 inhabitants, the national density is only 20.6.
- Furthermore, Human Resource for Health (HHR) distribution is uneven, with urban areas having a doctor density four times higher than in rural areas.
- There is nearly 80% shortage of specialist doctors at community health centres (CHCs) across rural India.
- While WHO recommends 44.5 doctors, nurses, and midwives per 10,000 inhabitants, the national density is only 20.6.
- Persistent Out-of-Pocket Healthcare Expenses and Insurance Gaps: Though reduced recently, high out-of-pocket expenses for healthcare services is still a significant burden for many Indians.
- Health insurance coverage in India is not as widespread as in countries like Germany, where health insurance is mandatory, leading to delayed or avoided treatments, which can result in further complications.
- India's insurance penetration fell to 3.7% in 2023-24 from 4% in the FY 2022-23.
- Although PM-JAY primarily covers inpatient hospitalization, it does not include outpatient and chronic care, which affects the affordability of treatment and hinders early intervention for various health conditions.
- The Comptroller and Auditor General (CAG) of India’s performance audit of the PM-JAY exposed significant irregularities, revealing critical implementation weaknesses.
- These shortcomings have, to some extent, left vulnerable beneficiaries underserved while contributing to increased health expenditure.
- The Comptroller and Auditor General (CAG) of India’s performance audit of the PM-JAY exposed significant irregularities, revealing critical implementation weaknesses.
- Health insurance coverage in India is not as widespread as in countries like Germany, where health insurance is mandatory, leading to delayed or avoided treatments, which can result in further complications.
- Insufficient Public Healthcare Expenditure: The Indian government's expenditure on healthcare has historically been low compared to other countries, which contributes to the inadequacy of public healthcare facilities and the high reliance on private healthcare services, which may not be affordable for all citizens.
- India’s public health expenditure stands at only 2.1% of GDP (2022-23), below the 2.5% recommended by the 15th Finance Commission.
- This limits the expansion of essential services, despite rising demand. In comparison, many developed countries allocate 5-10% of their GDP to health, highlighting India's challenge of underinvestment in the sector.
- India’s public health expenditure stands at only 2.1% of GDP (2022-23), below the 2.5% recommended by the 15th Finance Commission.
- Insufficient Focus on Preventive and Primary Healthcare: Healthcare in India continues to be predominantly focused on curative tertiary care, with less emphasis on prevention and primary health services.
- Non-communicable Diseases (NCDs) have been on the rise, putting additional strain on the healthcare system.
- The proportion of deaths due to NCDs in India has increased from 37.9% in 1990 to 61.8% in 2016.
- Non-communicable Diseases (NCDs) have been on the rise, putting additional strain on the healthcare system.
- Inadequate Focus on Mental Healthcare: Mental health remains an under-prioritized area within India’s healthcare system, with limited infrastructure, stigma, and low budget allocation.
- As per the National Mental Health Survey (2015–16), India has only 0.75 psychiatrists per 1 lakh population, far below the desirable standard of at least 3 per 1 lakh (recommended by WHO), leading to significant gaps in early diagnosis, treatment, and community-based support.
- Privacy Concerns Amid Growing Digitalisation: The growing use of digital tools in healthcare, such as electronic health records (Ayushman Bharat Health Account) and telemedicine, raises significant privacy concerns.
- The risk of unauthorized access to sensitive patient information, data breaches, and insufficient security measures can lead to the compromise of personal health data.
- In 2023, personal details of more than 80 crore people were leaked from the Indian Council of Medical Research (ICMR). This threatens patient confidentiality and undermines trust in the healthcare system.
- In 2022, AIIMS Delhi faced a massive ransomware attack posing critical vulnerabilities in India’s healthcare IT infrastructure.
- The risk of unauthorized access to sensitive patient information, data breaches, and insufficient security measures can lead to the compromise of personal health data.
What Strategies can India Adopt to Achieve Universal Health Coverage?
- Expand Universal Health Insurance to Holistically Cover Outpatient, Preventive, and Chronic Care: India can rethink PM-JAY and insurance schemes to encompass outpatient diagnostics, medicines, and preventive screenings, tackling the major share of out-of-pocket expenditure (only for the most vulnerable section in the initial stages).
- Introduce modular insurance products for chronic disease management, incentivizing early intervention and reducing hospitalization.
- This paradigm shift will ensure financial risk protection while aligning with global best practices for universal health coverage.
- Transform Health Workforce Capacity: Establish an incentive-based system that encourages healthcare professionals to serve in underserved areas through measures such as rural service bonds, fast-tracked career growth, and financial incentives.
- Additionally, medical education curricula should be aligned with community health needs, integrating training for multidisciplinary health workers, including AYUSH practitioners, through initiatives like the National Health Mission.
- This approach will foster a resilient, adaptable workforce capable of addressing India’s epidemiological transition and demographic diversity.
- Additionally, medical education curricula should be aligned with community health needs, integrating training for multidisciplinary health workers, including AYUSH practitioners, through initiatives like the National Health Mission.
- Create AI Enabled Digital Healthcare Infrastructure: India must prioritize the development of AI-ready infrastructure in healthcare facilities, ensuring stable electricity, strong internet connectivity, and the necessary hardware in healthcare centers.
- The government can leverage existing initiatives like the National Rural Health Mission to incorporate upgrades in digital infrastructure.
- A successful example is the solar-powered primary health centers in Chhattisgarh, which provide 24/7 electricity; this model can be expanded to include essential digital infrastructure.
- Further, integration of AI will help bridge the gap in healthcare access and delivery, improving efficiency and enabling better healthcare outcomes.
- The government can leverage existing initiatives like the National Rural Health Mission to incorporate upgrades in digital infrastructure.
- Strengthening Healthcare Connectivity through Digital Innovation: Government hospitals at all levels should be well-connected, particularly through digital platforms.
- This would facilitate the exchange of best practices, clinical protocols, and innovative solutions across the healthcare network, thereby elevating the overall standard of healthcare.
- Mobile Health Units with E-Health Integration can bridge healthcare access gaps in remote areas by providing medical services, ensuring timely care for underserved populations.
- Regular seminars and symposiums can be organized to foster a culture of knowledge sharing and continuous learning among healthcare providers.
- Unified Regulatory Framework for Private Healthcare with Digital Oversight: Create a centralized regulatory authority empowered to enforce comprehensive quality standards, ethical pricing, and grievance redressal across private providers.
- Integrate this framework with digital health initiatives such as ABDM and hospital accreditation bodies to enable real-time monitoring and transparency.
- Such harmonization will foster trust, reduce exploitative practices, and promote equitable healthcare delivery.
- Empowering Community Health Workers (CHWs): CHWs, such as ASHAs, are the frontline of India's health system. Instead of viewing them as mere volunteers, a transformative strategy is to professionally empower them.
- This involves providing them with better and more consistent salaries, not just performance-based incentives.
- Furthermore, they should be equipped with modern digital tools for data collection, telemedicine, and referral management, and be given an enhanced training curriculum that expands their roles to include screening for NCDs and basic mental health support.
- Drive Innovation and Self-Reliance in Pharmaceuticals and Medical Devices: Promote public-private partnerships and increase R&D funding for frontier technologies like organ bioprinting, robotics, and AI diagnostics under the Medical Device Policy 2023.
- Facilitate backward integration in supply chains and streamline regulatory approvals to bolster India’s global competitiveness.
- India can increase domestic production of Active Pharmaceutical Ingredients (APIs) to reduce reliance on imports, especially from China, which currently supplies around 70% of India's API requirements.
- Align these initiatives with the Make in India and Aatmanirbhar Bharat missions to transform India into a global hub for affordable, high-quality healthcare innovation.
- Facilitate backward integration in supply chains and streamline regulatory approvals to bolster India’s global competitiveness.
- Strengthening Mental Healthcare: India must urgently prioritize mental health by increasing dedicated funding and expanding mental healthcare infrastructure across the country.
- Strengthening the mental health workforce through the training and recruitment of more psychiatrists, psychologists, and counselors is essential to meet growing demand.
- Integrating mental health services into primary healthcare centers and community-based programs will enhance accessibility, promote early diagnosis, and ensure timely treatment.
- Initiatives like Tele-MANAS represent important advances in improving mental healthcare reach through digital platforms.
- Additionally, sustained public awareness campaigns are vital to reduce stigma and foster a culture that supports mental well-being, making mental health an integral part of India’s comprehensive healthcare system.
Conclusion
India stands at a pivotal moment in its journey towards achieving Universal Health Coverage (UHC) by 2030. While significant progress has been made, addressing the remaining challenges requires a comprehensive and forward-looking approach. The future of India’s healthcare lies in ensuring the 4 A's: Affordability, Accessibility, Availability, and Accountability. By prioritizing these pillars, India can build a healthcare system that is inclusive, equitable, and sustainable, ensuring that all citizens have access to quality healthcare services.
|
Drishti Mains Question What strategies should India adopt to achieve Universal Health Coverage (UHC) by 2030? Highlight key challenges and measures to address them. |
UPSC Civil Services Examination, Previous Year Questions (PYQs)
Prelims
Q. Which of the following are the objectives of ‘National Nutrition Mission’? (2017)
- To create awareness relating to malnutrition among pregnant women and lactating mothers.
- To reduce the incidence of anaemia among young children, adolescent girls and women.
- To promote the consumption of millets, coarse cereals and unpolished rice.
- To promote the consumption of poultry eggs.
Select the correct answer using the code given below:
(a) 1 and 2 only
(b) 1, 2 and 3 only
(c) 1, 2 and 4 only
(d) 3 and 4 only
Ans: (a)
Mains
Q. “Besides being a moral imperative of a Welfare State, primary health structure is a necessary precondition for sustainable development.” Analyse. (2021)