Governance
Transforming India’s Healthcare System
- 07 Jul 2025
- 23 min read
This editorial is based on “When government cares, healthcare makes strides” which was published in The Hindu on 07/07/2025. The article brings into picture the significant transformation of India’s healthcare system over the last 11 years, highlighting the National Health Mission’s role in establishing over 1.77 lakh Ayushman Arogya Mandirs.
For Prelims: National Health Mission, Ayushman Arogya Mandirs, Central Drugs Standard Control Organization, Medical Council of India, Insurance Regulatory and Development Authority of India, Ayushman Bharat Digital Mission, Medical Council of India.
For Mains: Regulation of Health Sector in India, Key Issues Associated with Indian Healthcare.
India's healthcare system has undergone a dramatic transformation over the past 11 years, evolving from a system plagued by infrastructure gaps and resource shortages to one focused on comprehensive, accessible care for all citizens. The National Health Mission has emerged as the cornerstone of this revolution, establishing over 1.77 lakh Ayushman Arogya Mandirs and leveraging digital platforms to democratize healthcare access across the country. This foundation positions India to achieve its ambitious vision of universal healthcare, marking a historic shift toward ensuring affordable, equitable, and quality healthcare reaches every corner of the nation.
What is the Current Structure of the Healthcare System in India?
- Primary Healthcare: Primary healthcare serves as the first point of contact for individuals seeking medical attention. It focuses on prevention, health education, and basic health services.
- Governance:
- State and District Level: Managed primarily by state governments through district health authorities and local governance bodies such as Panchayats.
- Service Providers: Primary Health Centres (PHCs), Sub-Centres, and Health and Wellness Centres (HWCs).
- Key Areas: Immunization, maternal and child health, outpatient care, prevention of common diseases like malaria, and health education.
- Governance:
- Secondary Healthcare: Secondary healthcare involves specialized medical care usually provided in district hospitals or regional centers.
- Governance:
- State Level: Managed by state governments via district and regional health authorities. Some specialized hospitals focus on certain conditions.
- Service Providers: District hospitals, Community Health Centres (CHCs), and Specialty Clinics.
- Governance:
- Tertiary Healthcare: Tertiary healthcare offers highly specialized services, usually for complex conditions that require advanced treatment.
- Governance:
- Central and State Governments: Managed by both central and state ministries. Major institutions such as AIIMS and PGIMER are under central governance.
- Service Providers: Specialized hospitals, medical colleges, and research institutions.
- Key Areas: Advanced treatment for diseases such as cancer, organ transplants, complex surgeries, and high-end diagnostics.
- Governance:
- Regulatory Bodies: India has multiple regulatory authorities to oversee various aspects of healthcare:
- Central Drugs Standard Control Organization (CDSCO): Regulates drugs, medical devices, and cosmetics in India, ensuring their safety, efficacy, and quality.
- Medical Council of India (MCI): Previously responsible for overseeing medical education and professional practice standards, though it has been replaced by the
- National Medical Commission (NMC) under the National Medical Commission Act, 2019. The NMC now regulates medical education, licensing, and professional ethics.
- Pharmacy Council of India (PCI): Regulates the education and practice of pharmacy in India, ensuring pharmacists meet required standards.
- National Accreditation Board for Hospitals and Healthcare Providers (NABH): Provides accreditation to hospitals and healthcare providers based on quality and safety standards.
- Insurance Regulatory and Development Authority of India (IRDAI): Regulates health insurance policies and ensures that they are fair and transparent for consumers.
- Key Healthcare Policies and Acts: The Indian government has enacted various laws and policies to regulate healthcare delivery:
- The Indian Medical Council Act (1956) and its successor, The National Medical Commission Act (2019), regulate medical practice and medical education standards.
- The Drugs and Cosmetics Act (1940): Regulates the import, manufacture, distribution, and sale of drugs and cosmetics in India.
- Clinical Establishments (Registration and Regulation) Act (2010): Provides a framework for the registration and regulation of healthcare establishments, ensuring quality healthcare standards in both public and private sectors.
- The Indian Nursing Council Act (1947): Regulates the education and practice of nurses and midwives.
- The National Health Policy (2017): Lays down the roadmap for the healthcare system in India, focusing on providing accessible, affordable, and quality healthcare services to all citizens.
- Recent Developments in Healthcare Regulation: India has made strides in healthcare regulations with the introduction of the Ayushman Bharat Digital Mission (ABDM), which aims to create a unified digital health ecosystem.
- The introduction of e-pharmacies is also being regulated by the government to ensure safe and legitimate online medical transactions.
- The regulation of telemedicine has also gained traction, with the Telemedicine Practice Guidelines released by the Medical Council of India (MCI) in 2020.
What are the Key Issues Associated with Indian Healthcare?
- Rural-Urban Healthcare Disparity: Despite significant strides in healthcare, India’s urban-rural divide remains a major challenge.
- The concentration of healthcare infrastructure in urban areas leaves rural populations underserved, with limited access to essential healthcare services.
- This gap exacerbates health inequities and delays treatment, worsening health outcomes.
- For example, rural areas often lack specialists, and the doctor-to-patient ratio in rural areas is much lower, impacting the quality of care.
- In 2022, over 80% of healthcare professionals were located in urban areas, while rural regions account for 68% of the population.
- Affordability of Healthcare: Affordability remains one of the most pressing concerns in India’s healthcare system, especially for low-income families.
- Despite initiatives like Ayushman Bharat, out-of-pocket expenditure (OOPE) continues to burden millions, leading to catastrophic health spending.
- The fee-for-service model, where patients pay for services even when insured, intensifies financial strain.
- In FY23, India's OOPE was still high at 47.1%, indicating the ongoing challenge in reducing health costs despite coverage schemes like PM-JAY, which insured over 10 crore families.
- Despite initiatives like Ayushman Bharat, out-of-pocket expenditure (OOPE) continues to burden millions, leading to catastrophic health spending.
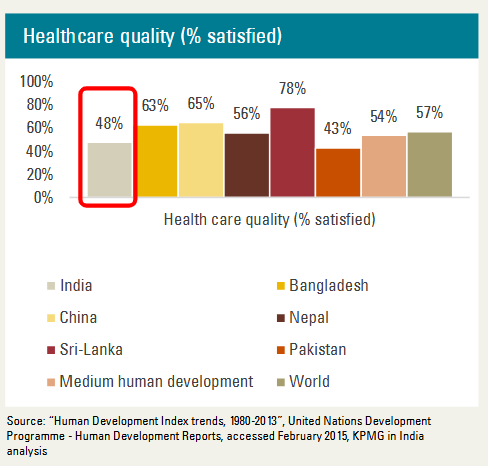
- Quality of Healthcare Services: Quality of care remains inconsistent across both public and private sectors, further challenging equitable healthcare access. Government hospitals, though affordable, suffer from outdated infrastructure, overcrowding, and staff shortages.
- Despite improving infrastructure, quality continues to be uneven, undermining patient trust in the public healthcare system.
- Also in the pharmaceutical sector, 1,394 batches of drugs, valued at more than ₹16.88 crore, were recalled during the FY 2023-24.
- As many as 3,053 drugs were found to be substandard during the financial year 2022-23.
- Non-Communicable Diseases (NCDs) Burden: The rising burden of non-communicable diseases (NCDs) like diabetes, cardiovascular diseases, and cancers is another critical issue.
- With lifestyle changes, India is witnessing an increase in NCDs, affecting both urban and rural populations.
- An estimated 5.8 million Indians die from NCDs each year, approximately one in four Indians faces the risk of dying from an NCD before reaching the age of 70.
- As per the NFHS-5 data, 23% of women and 22.1% of men in India are overweight as per the BMI criterion, indicating a growing public health crisis.
- Underutilization of Public Health Schemes: Despite government efforts to expand healthcare coverage, schemes like Ayushman Bharat still face issues in reach and utilization.
- Many eligible individuals in rural and underserved regions are unaware of these programs or face challenges in accessing them.
- CAG report on the Ayushman Bharat scheme reveals irregularities, including invalid mobile numbers and potential fraud.
- The CAG identified 4,761 registrations that were linked to only seven Aadhar numbers, indicating potential irregularities.
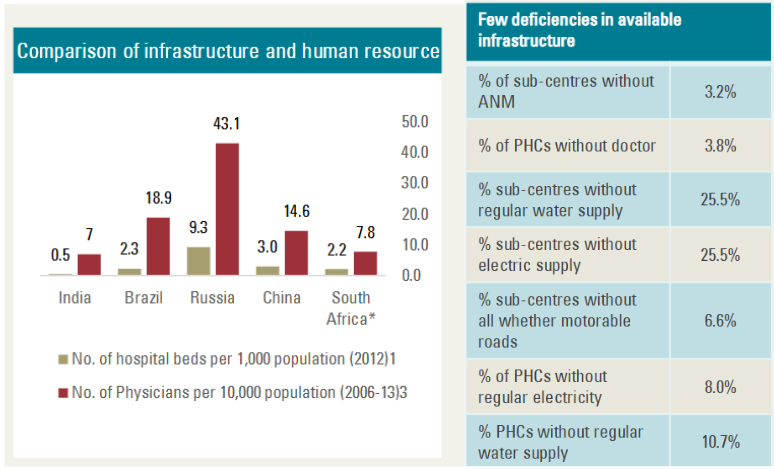
- Healthcare Infrastructure Gaps: While there have been improvements in healthcare infrastructure, India still faces major gaps, particularly in remote and underserved areas.
- Although more than 1.77 lakh Ayushman Arogya Mandirs were established, healthcare facilities remain underdeveloped, with inadequate equipment, personnel, and services.
- Health Insurance Penetration: Although health insurance penetration has increased significantly, millions remain uninsured, especially in the informal sector.
- The rise in medical insurance premiums and high out-of-pocket costs for consultations, diagnostics, and drugs continue to hinder access.
- Insurance penetration in India is among the lowest in the world. Measured as a ratio of annual premium to the country's gross domestic product (GDP), insurance penetration declined from 4% in 2022-23 to 3.7% in 2023-24, according to the Insurance Regulatory and Development Authority.
- Regulation of Private Healthcare Sector: While private healthcare provides high-quality services, it is largely unregulated, resulting in high costs and inconsistent care.
- The absence of strong regulations allows private hospitals to operate with minimal accountability, often charging exorbitant rates for essential services.
- India has nearly twice as many private hospitals as public ones and 70% of the population prefer to seek healthcare from private sector hospitals often at hefty charges.
What Measures can India Adopt to Enhance the Healthcare Sector?
- Strengthening Primary Healthcare through Integrated Models: India must expand and strengthen its primary healthcare infrastructure by promoting an integrated model that combines preventive, curative, and palliative care.
- This can be achieved by enhancing Ayushman Bharat Health and Wellness Centres (HWCs), ensuring they are equipped with the latest medical technologies and staffed with trained professionals.
- A more cohesive primary care system can reduce the strain on secondary and tertiary care hospitals, ensuring early intervention and reducing long-term healthcare costs.
- Accelerating Health Workforce Training and Deployment: To address the acute shortage of healthcare professionals, India must focus on not only increasing the number of medical schools but also improving training programs to ensure quality healthcare providers across the country.
- Specialized training for Community Health Officers (CHOs) should be ramped up to bridge the gap between primary healthcare workers and medical officers.
- Additionally, incentivizing healthcare professionals to serve in underserved rural areas through financial benefits and career development opportunities could improve the distribution of healthcare workers.
- Leveraging Telemedicine and Digital Health Platforms: Telemedicine and digital health platforms should be fully integrated into the mainstream healthcare system to provide affordable and accessible care, especially in rural areas.
- India can establish a robust telemedicine framework through collaborations with private and non-profit organizations, while enhancing platforms like eSanjeevani.
- This would allow for virtual consultations, digital prescriptions, and better management of chronic diseases, while reducing the burden on physical healthcare facilities.
- Public-Private Partnerships to Expand Infrastructure: To close the infrastructure gap, India should increase the use of public-private partnerships (PPPs) to scale up the construction and maintenance of healthcare facilities.
- The government can incentivize private sector investments by offering tax rebates and easing regulations for healthcare providers willing to build in underserved areas.
- PPPs can enhance the quality of care in district hospitals, establish specialized centers in rural areas, and ensure the availability of advanced medical equipment without relying solely on government funding.
- Reforming Health Insurance to Achieve Universal Coverage: India must expand and reform its health insurance systems to ensure that universal healthcare is accessible to all, including the informal sector.
- Simplifying insurance schemes like Ayushman Bharat and expanding their scope to cover outpatient services and diagnostic procedures would make healthcare more affordable.
- The government should also focus on making insurance premiums more affordable and creating awareness about these schemes, particularly in rural areas where awareness and access remain low.
- Emphasizing Preventive and Wellness Care: Shifting the focus of healthcare from treatment to prevention is critical. India should launch nationwide campaigns to raise awareness about lifestyle diseases, encourage regular screenings, and promote healthy habits through digital platforms and local healthcare initiatives.
- Building a robust national framework for preventive care through partnerships with schools, communities, and workplaces would significantly reduce the burden of non-communicable diseases (NCDs) and lower healthcare costs over the long term.
- Strengthening Healthcare Financing Mechanisms: To ensure sustainable healthcare delivery, India needs to enhance its healthcare financing mechanisms, targeting an increase in public expenditure on health to at least 2.5% of GDP.
- This could be achieved through reallocation of existing resources, improving the efficiency of public health spending, and encouraging private sector contributions through targeted incentives.
- Additionally, creating specialized healthcare bonds or setting up healthcare innovation funds could attract investments into the sector, ensuring long-term financial stability.
- Improving Regulatory Framework for Private Healthcare: India must establish a stronger regulatory framework for the private healthcare sector to ensure transparency, affordability, and quality of care.
- This includes standardizing medical pricing across private institutions, establishing clear guidelines for ethical practices, and regulating the cost of essential services.
- Integration of Traditional and Modern Medicine: India can integrate traditional medicine like Ayurveda, Homeopathy, and Siddha into the mainstream healthcare system, creating a holistic approach to health.
- By setting standards for these practices and ensuring their integration with modern medical care, the country can offer a broader range of affordable, culturally relevant healthcare options.
- This would also alleviate pressure on conventional healthcare systems while preserving India’s rich medical heritage.
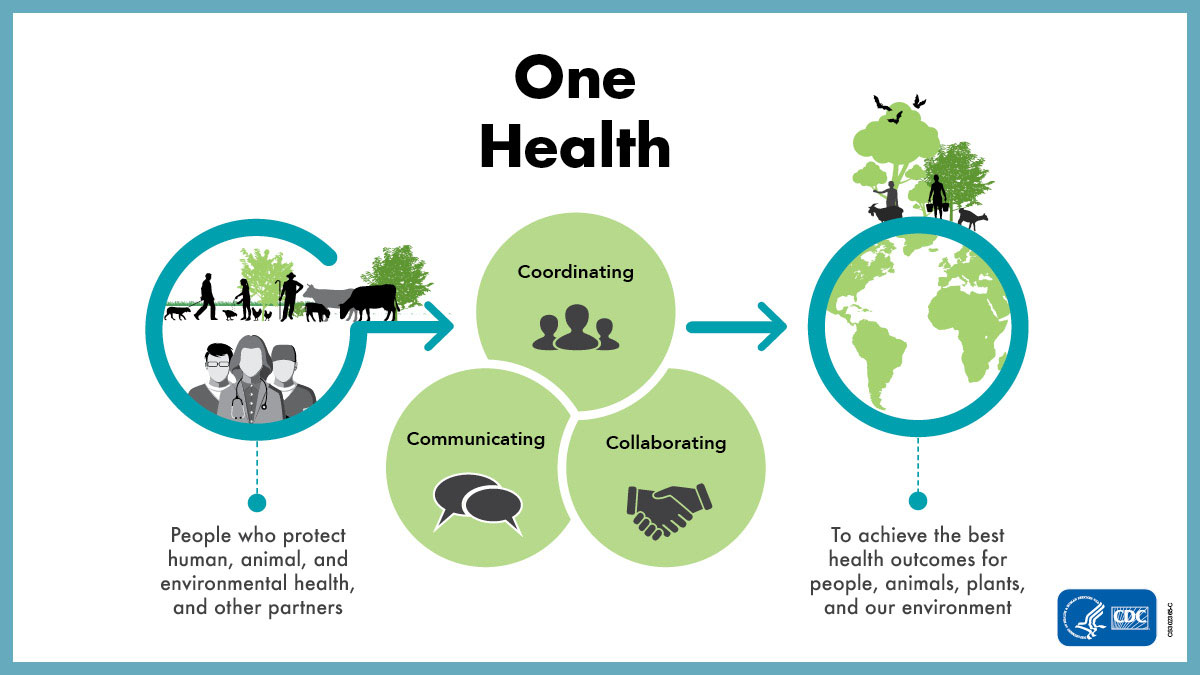
- India should also enhance focus on One Health Approach.
- Fostering Healthcare Innovation through Startups and Technology: India should actively foster innovation in healthcare through the creation of incubators and accelerators dedicated to health-tech startups.
- Encouraging collaborations between tech innovators, research institutions, and healthcare providers can lead to the development of cost-effective, scalable solutions such as AI-based diagnostics, wearable health devices, and personalized medicine.
- Government grants and venture capital funding for these startups will drive the next wave of technological advancements in healthcare, improving access and affordability for all citizens.
What India can Learn from Other Countries to Improve its Healthcare Sector?
- Universal Healthcare Models (UK): India can learn from the UK's National Health Service (NHS) which provide universal healthcare funded through taxes.
- These systems ensure that healthcare is free or low-cost at the point of use, reducing out-of-pocket expenses and promoting equity.
- Primary Healthcare Focus (Brazil): Brazil's Family Health Program has significantly improved access to primary healthcare by deploying community health workers in underserved areas.
- India can adopt this approach by strengthening its Health and Wellness Centres (HWCs) and training more Community Health Officers (CHOs) to improve healthcare delivery in rural regions, focusing on prevention and early intervention.
- Digital Health Integration (Estonia): Estonia’s advanced digital health infrastructure, including e-health records and telemedicine, offers a streamlined approach to healthcare management.
- India can integrate similar digital systems to enhance efficiency, improve patient care coordination, and reduce administrative costs.
- Expanding platforms like eSanjeevani nationwide could facilitate remote consultations and improve healthcare access.
- Public-Private Partnerships (Singapore): Singapore has successfully leveraged public-private partnerships (PPPs) to build world-class healthcare infrastructure.
- India can enhance its healthcare system by fostering similar collaborations to expand hospital capacity, modernize facilities, and improve the quality of care, especially in rural and underserved regions.
- Preventive Healthcare Emphasis (Japan): Japan’s focus on preventive healthcare through regular screenings, health education, and public awareness campaigns has resulted in high life expectancy and low disease burden.
- India can adopt a stronger emphasis on prevention by integrating regular health check-ups and awareness programs into its public health initiatives to reduce the burden of non-communicable diseases (NCDs).
Conclusion:
India's healthcare system is undergoing significant transformation with a focus on universal access, quality care, and digital integration. Strengthening primary healthcare, expanding insurance coverage, and fostering public-private partnerships are crucial to bridging these gaps. Aligning these efforts with the UN's SDG 3 (Good Health and Well-Being) and the recently released Global Pandemic Treaty will be key to ensuring sustainable, equitable healthcare for all.
|
Drishti Mains Question: Discuss the transformation of India’s healthcare system over the past decade, highlighting key regulatory reforms, infrastructural challenges, and the role of digital platforms in ensuring equitable healthcare access. |
UPSC Civil Services Examination, Previous Year Questions (PYQs)
Prelims
Q. Which of the following are the objectives of ‘National Nutrition Mission’? (2017)
- To create awareness relating to malnutrition among pregnant women and lactating mothers.
- To reduce the incidence of anaemia among young children, adolescent girls and women.
- To promote the consumption of millets, coarse cereals and unpolished rice.
- To promote the consumption of poultry eggs.
Select the correct answer using the code given below:
(a) 1 and 2 only
(b) 1, 2 and 3 only
(c) 1, 2 and 4 only
(d) 3 and 4 only
Ans: (a)
Mains
Q. “Besides being a moral imperative of a Welfare State, primary health structure is a necessary precondition for sustainable development.” Analyse. (2021)