Social Justice
India’s Battle Against Tuberculosis
- 16 May 2025
- 11 min read
For Prelims: Tuberculosis, World Health Organization, Ayushman Arogya Mandirs, Ni-kshay Poshan Yojana
For Mains: National Tuberculosis Elimination Programme, Health and Disease Control
Why in News?
The Prime Minister chaired a high-level review meeting on the National Tuberculosis Elimination Programme (NTEP) and emphasized the need for targeted, data-driven interventions and the use of technology to accelerate India’s mission to eliminate tuberculosis (TB) by 2025.
National TB Elimination Programme (NTEP)
- NTEP: In 2020, the Revised National Tuberculosis Control Program (RNTCP) was renamed the NTEP with the goal to eliminate TB in India by 2025, five years ahead of the global target of 2030.
- The Sustainable Development Goal targets for TB include 80% reduction in incidence, 90% reduction in mortality, and zero TB patients facing catastrophic costs.
- The program is guided by the National Strategic Plan (2017-2025) under the strategic pillars: Detect – Treat – Prevent – Build (DTPB).
- The NTEP focuses on early diagnosis, quality-assured treatment, engaging private providers, contact tracing in high-risk areas, and addressing social determinants through a multi-sectoral approach.
- The programme recorded its highest-ever case notifications, reporting 25.5 lakh TB cases in 2023 and 26.07 lakh cases in 2024.
- Under NTEP, India introduced improved drug-resistant TB treatments, including a safer, shorter all-oral Bedaquiline regimen, increasing success rates from 68% in 2020 to 75% in 2022.
- The mBPaL regimen (Bedaquiline, Pretomanid, Linezolid) offers 80% success for MDR-TB, reducing treatment duration to six months.
- Pradhan Mantri TB Mukt Bharat Abhiyaan (PMTBMBA): Launched in 2022 as part of NTEP, it focuses on providing nutritional, diagnostic, and vocational support to improve treatment outcomes and accelerate India's TB elimination goal. P
- PMTBMBA is the world’s largest crowd-sourcing initiative for TB patient nutrition.
- The Ni-Kshay Mitra initiative, part of the PMTBMBA, encourages individuals, NGOs, and corporations to support TB patients with nutritional, social, or economic aid for six months.
- The Ni-Kshay Portal helps health workers manage TB cases, track treatment, and report real-time data for India's TB surveillance.
What Progress has India made under the National TB Elimination Programme?
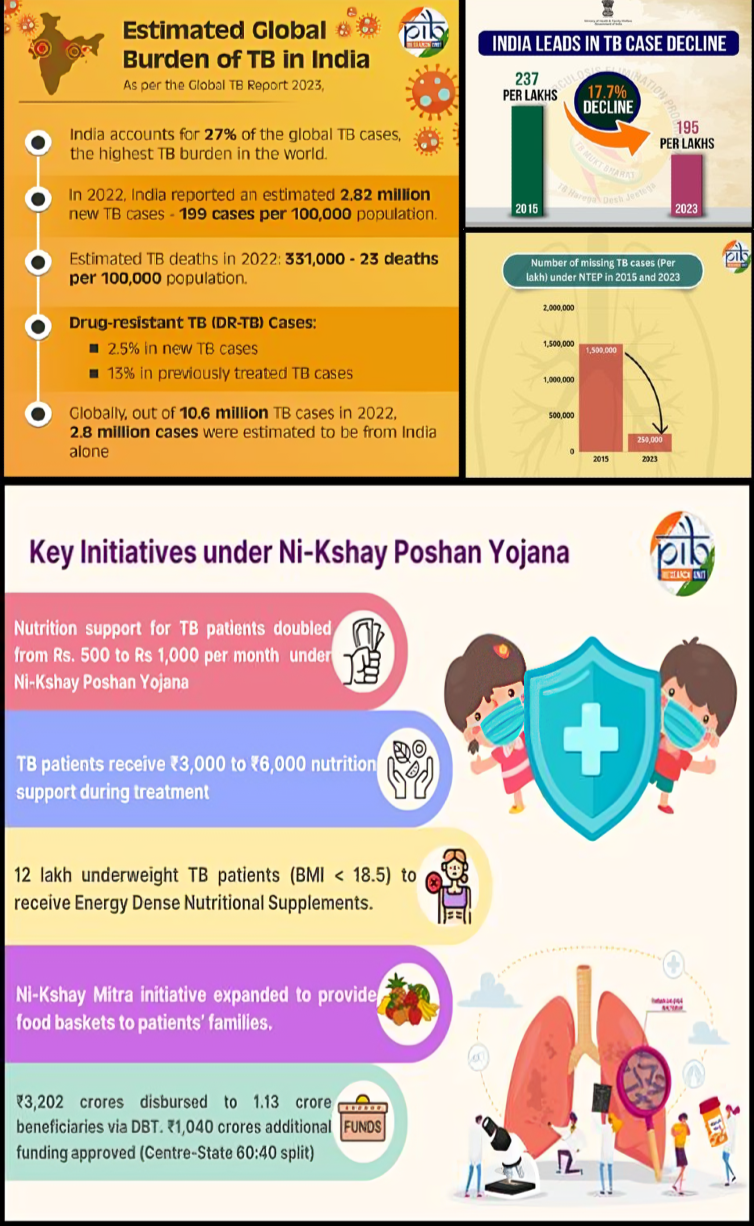
- Reduction in TB Incidence and Mortality: The World Health Organization (WHO) Global TB Report 2024 highlighted that TB incidence in India declined by 18% (from 237/lakh in 2015 to 195/lakh in 2023), over double the global decline of 8%.
- TB mortality reduced by 21%, from 28 to 22 deaths per lakh population.
- In 2023, India alone accounted for over 26% of global TB cases and deaths.
- Increased Treatment Coverage: TB treatment coverage has risen to 85%, reflecting the success of NTEP strategies and decentralized care through 1.7 lakh Ayushman Arogya Mandirs.
- 100-Day TB Mukt Bharat Abhiyaan: During 100-Day TB Mukt Bharat Abhiyaan campaign, 12.97 crore individuals were screened in high-focus districts, leading to the detection of 7.19 lakh TB cases, including 2.85 lakh asymptomatic cases.
- Nikshay Mitra Initiative: 2.55 lakh Nikshay Mitras (volunteers) have supported TB patients, distributing 29.4 lakh nutrition baskets to patients, demonstrating the role of community participation in the elimination efforts.
- Ni-kshay Poshan Yojana: The Ni-kshay Poshan Yojana has facilitated Direct Benefit Transfer (DBT) payments to 1.28 crore TB patients since 2018.
- The incentive amount for nutritional support has been enhanced to Rs 1,000 in 2024, promoting better health outcomes for patients undergoing TB treatment.
- Expansion of Diagnostic Infrastructure: India has significantly expanded its TB diagnostic network with NAAT (Nucleic Acid Amplification Testing) labs (helps in the detection of TB) and drug susceptibility labs, and deployed AI-enabled X-ray units enhancing accessibility and early detection.
- Screening has expanded to high-risk settings like mines, construction sites, tea gardens, and urban slums to identify cases in vulnerable populations.
What are the Key Facts About Tuberculosis?
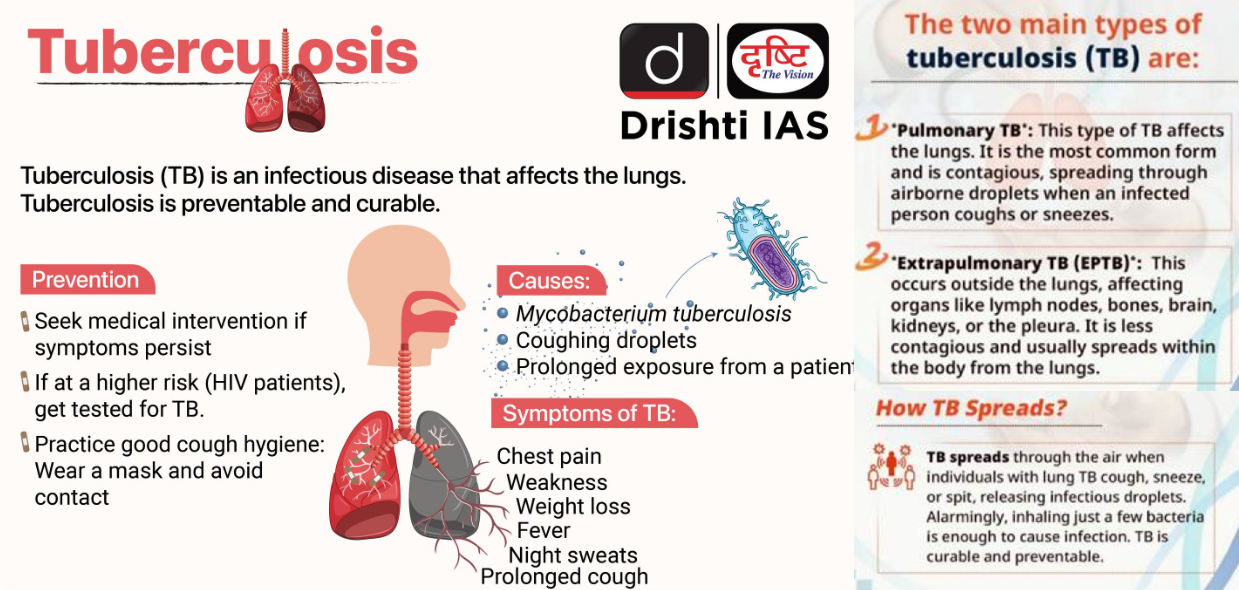
- About: TB is a bacterial infection (Mycobacterium tuberculosis) affecting the lungs, spreading through the air. It is preventable and curable with antibiotics.
- About 25% of the global population is infected, but only 5–10% develop symptoms.
- Risk Factors: Weak immune system, diabetes, malnutrition, tobacco, and alcohol use.
- Diagnosis: WHO recommends rapid molecular diagnostic tests as initial tests for people showing signs and symptoms of TB. Other diagnostic tools can include sputum smear microscopy and chest X-rays.
- Prevention: The Bacille Calmette-Guérin (BCG) vaccine is given to infants to prevent TB.
- Transmission: TB spreads through the air when an infected person coughs, sneezes, or spits, releasing germs that others can inhale.
- Treatment: Standard TB treatment lasts 4-6 months. Incomplete treatment leads to drug-resistant TB.
- Multidrug-resistant TB (MDR-TB): It is resistant to isoniazid and rifampicin (medicines used to treat TB), treatable with costlier alternatives.
- Extensively Drug-Resistant TB: It is more severe, with limited treatment options.
- TB and Human Immunodeficiency Virus (HIV): HIV patients are 16 times more vulnerable to TB, a leading cause of their deaths.
What Challenges do Vulnerable Groups face While Battling TB?
- Inadequate Nutrition: Undernutrition is a critical risk factor that both increases susceptibility to TB infection and worsens treatment outcomes.
- Vulnerable groups often lack sufficient nutritional support, which leads to higher mortality rates, increased drug toxicity, and relapse.
- Although government schemes exist (such as the Nikshay Poshan Yojana and Ni-kshay Mitras), the reach and effectiveness of nutritional aid remain limited.
- Delayed and Missed Diagnosis: Symptoms of TB are often mistaken for common ailments among the poor, leading to delayed diagnosis.
- Women, particularly homeless women, face longer delays than men in reaching diagnosis due to stigma, lack of awareness, and difficulty accessing health facilities.
- Diagnostic procedures like sputum collection are uncomfortable or inaccessible, especially for women who face cultural barriers.
- Social Stigma and Isolation: TB carries significant stigma, which discourages patients, especially women, from seeking timely treatment.
- The NTEP does not specifically recognize homelessness as a vulnerability category, resulting in gaps in data collection and tailored interventions.
- Homeless individuals face marginalization and social exclusion and often lack official documents like Aadhar cards and bank accounts, which are essential for accessing government schemes and financial support, further worsening their health and diminishing their motivation or ability to seek care.
- Childhood TB: It is difficult to diagnose due to low bacterial load, inability of young children to produce sputum, reliance on less sensitive tests like smear microscopy and chest X-rays, and limited drug resistance screening.
- Only 12% of molecular tests in children confirmed TB bacteriologically in 2022.
- Mental Health and Psychosocial Support Deficits: Mental health challenges related to TB diagnosis and treatment are often neglected, leaving patients without adequate psychological support, which can affect treatment success.
How can Targeted Interventions Help in TB Elimination?
- Implement Urban-Rural and Occupational Analysis: Analyzing TB patient data based on urban-rural and occupational distinctions to identify vulnerable groups, particularly workers in high-risk sectors like construction, mining, and textiles.
- Tailored interventions will help ensure early testing and effective treatment for these at-risk populations, reducing disease spread in high-risk environments.
- Including homeless populations as a vulnerable group in NTEP will ensure they get prioritized screening and treatment, overcoming barriers like lack of ID, stigma, and limited healthcare access.
- Encourage Public Participation (Jan Bhagidari): Public participation in the fight against TB, highlighted by Nikshay Mitra volunteers, is crucial for reducing stigma, increasing awareness of TB’s curability, and promoting support to eliminate the disease.
- Reducing Transmission Hotspots: Concentrating efforts in high-incidence areas or congregate settings like tea gardens, construction sites, and mines can break the chain of infection.
- Early Detection & Diagnosis: Deploying molecular diagnostic tools like NAAT and AI-based X-rays in vulnerable areas leads to faster, more accurate diagnosis, especially in hard-to-detect childhood and drug-resistant TB cases.
Conclusion
India’s TB elimination by 2025 remains challenging, but targeted, data-driven interventions, improved diagnostics, and strong community support offer a clear path forward. Early detection and focused efforts in high-risk groups are key to ending TB.
|
Drishti Mains Question: India has set an ambitious target of eliminating tuberculosis (TB) by 2025. Discuss the progress made under the National TB Elimination Programme. |
UPSC Civil Services Examination, Previous Year Questions (PYQs)
Mains
Q. “Besides being a moral imperative of a Welfare State, primary health structure is a necessary precondition for sustainable development.” Analyse. (2021)