Governance
The Burden of Non-communicable Diseases (NCDs) in India
This editorial is based on “ India’s burden of lifestyle diseases is growing. We need a multi-pronged approach”, which was published in The Indian Express on 17/10/2025. The article highlights that India’s growing lifestyle disease burden, including heart disease, diabetes, and respiratory disorders, requires an integrated national approach combining healthcare, nutrition, environment, prevention, and grassroots diagnostics.
For Prelims: Non-communicable diseases (NCDs), 2017 National Health Policy, Chronic Obstructive Pulmonary Disease (COPD), National Programme for Prevention and Control of Non-Communicable Diseases (NP-NCD), Ayushman Bharat Health and Wellness Centres (AB-HWCs), National Tobacco Control Programme (NTCP), National Nutrition Mission (POSHAN Abhiyaan), Fit India Movement.
For Mains: Recent Trends in the Burden of Non-communicable Diseases (NCDs) in India, Key Factors Contributing to the Rising Burden of Non-communicable Diseases (NCDs) in India, Strategies to Effectively Control the Rising Burden of Non-communicable Diseases in India
The 2017 National Health Policy underscored the alarming rise of non-communicable diseases (NCDs) such as heart disease, diabetes, and respiratory disorders, a trend that the latest Global Burden of Disease study shows has intensified over the past eight years. Despite advances in healthcare, gaps in early detection, public awareness, and preventive measures persist, compounded by lifestyle and environmental factors. Tackling this challenge demands a comprehensive, multi-pronged strategy that combines medical care, community education, and coordinated policy action to protect health and improve quality of life.
What are the Recent Trends in the Burden of Non-communicable Diseases (NCDs) in India?
- Dominance of NCDs in Mortality: Non-communicable diseases (NCDs) are medical conditions or diseases that are not caused by infectious agents and usually have a long duration and slow progression.
- NCDs such as cardiovascular diseases, diabetes, cancer, and chronic respiratory ailments now account for nearly 63–65% of all deaths in India, rising from 37.9% in 1990 to over 63% by 2023.
- This reflects a continuing epidemiological shift away from infectious diseases toward chronic conditions driven by lifestyle and demographic changes.
- High Rate of Premature Mortality: Approximately 25–26% of NCD-related deaths occur between ages 30 and 70, indicating a severe loss in prime productive years.
- Early Onset and Youth Vulnerability: According to the 10th International Diabetes Federation (IDF) Atlas, 2021, India has 2,294,000 children aged 0–19 years living with type 1 diabetes.
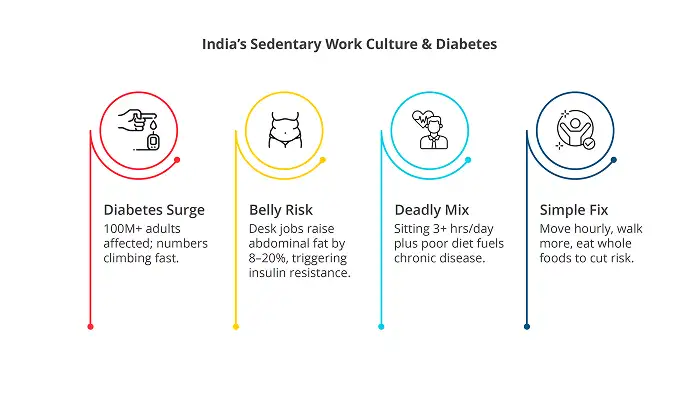
- Experts link this to sedentary behaviour, processed diets, and early-life nutritional deficiencies.
- Growing Economic and Social Burden: India is projected to lose $4.58 trillion by 2030 due to non-communicable diseases (NCDs) and mental health conditions. Among these, cardiovascular diseases will contribute $2.17 trillion, while mental health conditions will account for $1.03 trillion in economic losses.
- NCDs reduce quality of life, cause disabilities, and strain middle-aged working populations, directly affecting India’s demographic dividend.
What Are the Key Factors Contributing to the Rising Burden of Non-Communicable Diseases (NCDs) in India?
- Triple Burden of Malnutrition: India faces a paradoxical coexistence of undernutrition, micronutrient deficiencies, and obesity, intensifying metabolic disorders.
- Obesity now surpasses underweight as a public health concern.
- According to NFHS-5, the prevalence of overweight and obesity has increased significantly: 44% among men and 41% among women, compared to earlier surveys.
- The economic impact of obesity in India was $28.95 billion (Rs 2.4 lakh crore) in 2019, accounting for 1.02% of GDP.
- It is projected to rise to $81.53 billion (Rs 6.7 lakh crore) by 2030 (≈1.57% of GDP) and could soar to $838.6 billion (Rs 69.6 lakh crore) by 2060, or 2.5% of GDP, if unchecked.
- Sedentary lifestyles and Dietary Changes: Rapid urbanisation is reshaping food consumption patterns across India.
- The shift to processed, calorie-rich foods high in fats, sugars, and salt has increased dramatically, especially in urban and peri-urban areas.
- This "nutrition transition" is linked to rising obesity rates.
- Sedentary lifestyles affect over 31% of adults and 80% of adolescents (WHO), driven by increased mechanisation, screen time, and urban work patterns.
- Insufficient access to recreational spaces and safe urban design compounds physical inactivity.
- The shift to processed, calorie-rich foods high in fats, sugars, and salt has increased dramatically, especially in urban and peri-urban areas.
- High Tobacco and Substance Use: Tobacco use remains a major driver of NCDs, with nearly 28% of adults using some form of tobacco, including smoking and smokeless types.
- In 2021, tobacco was estimated to be the 5th highest risk factor contributing to deaths and disability combined in India.
- Tobacco causes about 1 in 5 male deaths and 1 in 20 female deaths in India.
- Similarly,harmful alcohol use and stress due to social inequities further elevate NCD risk.
- Air Pollution as a Major Risk Factor: According to the Global Burden of Disease (GBD) 2023 Report , air pollution remains among India’s top three causes of premature death and disability.
- According to the State of Global Air 2024, air pollution causes over 2 million deaths annually in India.
- Chronic Obstructive Pulmonary Disease (COPD) accounts for 75% of chronic respiratory diseases, heavily linked to indoor cooking fuel smoke and urban ambient pollution.
- With millions exposed daily to particulate matter above safe limits, the pollution–NCD link exacerbates respiratory and cardiac morbidity.
- Mental Health Disorders: Mental health conditions have sharply increased in India over the last decade.
- Anxiety disorders rose by 63%, and depression by 26% from 2013 to 2023.
- Psychological distress worsens NCD outcomes by affecting lifestyle adherence and exacerbating biological responses such as hypertension, necessitating integrated physical and mental health services.
- Healthcare System Gaps and Inequities: India’s vast rural areas face inadequate diagnostic and treatment facilities.
- While government schemes like the National Programme for Prevention and Control of NCDs (NP-NCD) exist, early detection and management are hindered by limited infrastructure and workforce shortages, especially in tribal and underserved regions.
- Disease burden varies up to tenfold among states, highlighting health inequities aggravated by socioeconomic disparities.
What are the Major Government Initiatives Aimed at Preventing and Controlling Non-communicable Diseases (NCDs) in India?
- National Programme for Prevention and Control of Non-Communicable Diseases (NP-NCD): Launched in 2010 and recently expanded, NP-NCD targets key NCDs like cardiovascular diseases, diabetes, cancer, chronic respiratory illnesses, and stroke.
- The program integrates population-based screening for individuals over 30, including opportunistic screening at all healthcare facilities.
- By 2025, under the nationwide “75/25 initiative,” 42 million hypertensive and 25 million diabetic patients have been treated, achieving nearly 90% of its target.
- The program also leverages teleconsultations and a dedicated National NCD Portal for monitoring. However, infrastructural gaps remain challenging in rural and tribal areas.
- Ayushman Bharat Health and Wellness Centres (AB-HWCs): With 1.5 lakh operational centres as of December 2022, AB-HWCs provide comprehensive primary healthcare, including NCD screening and wellness activities across all age groups.
- National Tobacco Control Programme (NTCP): NTCP deploys awareness campaigns, enforcement of tobacco legislation, and cessation support to reduce tobacco prevalence, which remains at 28.6% among adults despite prior reductions.
- Special focus is placed on youth tobacco use, a critical risk factor for NCDs.
- National Mental Health Programme (NMHP): Recognising the connection between mental health and NCDs, NMHP integrates mental health services within primary care to address rising anxiety and depression, which worsen physical illnesses and complicate NCD treatment adherence.
- National Nutrition Mission (POSHAN Abhiyaan): Beyond undernutrition, the mission tackles micronutrient deficiencies and rising obesity, emphasizing early-life nutrition to reduce future metabolic disorders.
- National Clean Air Programme (NCAP): Addressing air pollution as a major NCD risk factor, NCAP implements measures to improve air quality, essential for lowering respiratory and cardiovascular diseases associated with polluted environments.
- Specialized Ayurvedic Care: The All India Institute of Ayurveda (AIIA) in New Delhi offers specialized treatments for obesity and related lifestyle disorders, combining Panchakarma therapies, Ayurvedic medications, personalized dietary guidelines, and yoga therapy.
- Eat Right India Movement (FSSAI): The Eat Right India movement, initiated by the Food Safety and Standards Authority of India (FSSAI), includes several initiatives to ensure safe, healthy, and sustainable food for all.
- Fit India Movement: Launched in 2019, the Fit India Movement promotes active lifestyles and encourages daily physical fitness.
- Fit India School Certification for schools integrating physical activity into the curriculum.
- Fit India Sundays on Cycle initiative, promoting cycling and walking in urban spaces.
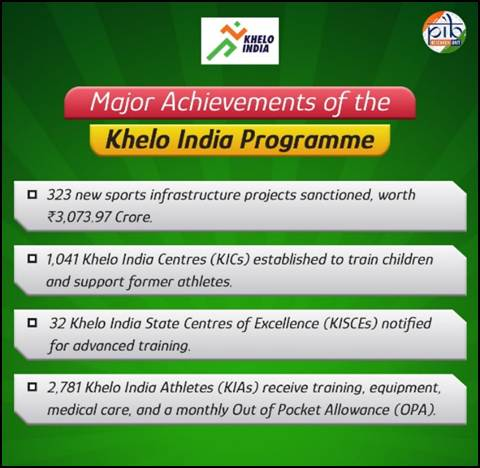
- Khelo India – National Programme for Development of Sports:Launched in 2016-17, the Khelo India programme fosters sports participation from schools to elite competitions, promoting a culture of athletic excellence.
- It provides top-notch training and world-class infrastructure to young athletes, ensuring equal sports opportunities across rural and urban India.
What Comprehensive Strategies can India adopt to Effectively Control the Rising Burden of Non-communicable Diseases?
- Strengthen and Scale Up National NCD Screening and Management Programs: Emphasise effective implementation of the National Programme for Prevention and Control of Non-Communicable Diseases (NP-NCD) aims to screen all individuals aged 30 and above for hypertension, diabetes, oral, breast, and cervical cancers, targeting a total of 50 crore people by 2025.
- Its continuous integration with Ayushman Bharat Health and Wellness Centres (AB-HWCs) will enhance the accessibility of screening and follow-up services.
- The use of digital tools such as the National NCD Portal and teleconsultation services (e-Sanjeevani) will improve both monitoring and access.
- Implement Multi-sectoral Policy Responses: Prioritize implementation of India’s National Multi-sectoral Action Plan (NMAP) for NCDs which emphasises coordination across ministries such as Health, Environment, Finance, Education, and Commerce.
- The plan sets targets including the reduction of tobacco use by 30%, alcohol use by 10%, and salt intake by 30% by 2025.
- Promoting policies like ‘Health-in-All-Policies’ approach will help preventing policy conflicts and regulating commercially-driven risk factors including tobacco, alcohol, and junk food.
- Expand Community Engagement and Capacity-building: Accredited Social Health Activists (ASHAs) and Community Health Officers (CHOs) are empowered to conduct door-to-door NCD screening, counselling, and monitoring.
- Proper training of CHOs and frontline workers in early diagnosis and patient follow-up is crucial to improving coverage and quality of care.
- Community awareness campaigns, such as the Fit India Movement and Eat Right India, promote behavioural changes in physical activity and nutrition.
- Integrate Mental Health with NCD Care: The National Mental Health Programme (NMHP) is being expanded to address anxiety, depression, and substance abuse, which negatively impact NCD outcomes.
- Screening for mental health disorders at NCD clinics and the provision of counselling services will ensure a more holistic approach to care.
- Strengthen Infrastructure and Supply Chains: District-level strengthening is essential, including the establishment and upgrading of Day Care Cancer Centres (DCCCs) in district hospitals to provide accessible oncology services, as planned in Budget 2025-26.
- It is necessary to ensure the uninterrupted supply of essential drugs and diagnostics at all healthcare levels.
- Additionally, improving tertiary care infrastructure and referral systems is important for handling complicated cases.
- Leverage Technology and Data-driven Approaches: The expansion of digital health solutions, such as AI for risk prediction, teleconsultations, and digital registries, enhances early detection, follow-up, and adherence to treatment.
- The National NCD Portal should be regularly updated and used for facility monitoring and policy decisions.
- Furthermore, promoting research on innovative care models and cost-effective interventions helps develop solutions suitable for resource-constrained settings.
- Address Environmental and Social Determinants: Programs like the National Clean Air Programme (NCAP) are being implemented and enforced to reduce ambient and indoor air pollution, which is a major driver of respiratory and cardiovascular NCDs.
- The creation of safe urban spaces should be promoted to encourage physical activity.
- Policies that reduce socioeconomic inequities in access to prevention and care improve health outcomes among vulnerable populations.
Conclusion :
Tackling non-communicable diseases (NCDs) requires a comprehensive, multi-sectoral approach that goes beyond the health sector, integrating efforts across nutrition, education, environment, and community welfare. The way forward lies in strengthening primary healthcare, leveraging technology, promoting healthy lifestyles, and ensuring equitable access to quality care—paving the path toward a healthier and more resilient India. As Prime Minister Shri Narendra Modi aptly remarked, “By making small changes in our food habits, we can make our future stronger, fitter, and disease-free,” a vision that perfectly embodies India’s collective fight against NCDs.
|
Drishti Mains Question: As India transitions from communicable to lifestyle diseases, the challenge is not of infection but of inaction. Examine how India’s health policies are adapting to address the growing burden of Non-Communicable Diseases (NCDs) in a rapidly urbanising society. |
Frequently Asked Questions (FAQs)
1. What is the current burden of non-communicable diseases (NCDs) in India?
NCDs cause 63–65% of deaths in India, up from 37.9% in 1990, indicating a shift toward chronic diseases.
2. What are the key lifestyle and environmental factors driving the rise of NCDs in India?
Unhealthy diets, sedentary lifestyles, tobacco/alcohol use, air pollution, and early-life nutritional deficiencies.
3 .Which major government programs address NCD prevention and control in India?
National Programme for Prevention and Control of Non-Communicable Diseases (NP-NCD), Ayushman Bharat Health and Wellness Centres (AB-HWCs), National Tobacco Control.
4. How is India strengthening NCD screening and management?
Screening all 30+ individuals, AB-HWC integration, digital tools, teleconsultations, targeting 50 crore people by 2025.
5. What comprehensive strategies are recommended to control NCDs in India?
Multi-sectoral policies, community engagement, mental health integration, stronger infrastructure, tech-driven monitoring, and reducing social/environmental risks.
UPSC Civil Services Examination Previous Year Question (PYQ)
Prelims
Q. Which of the following diseases can be transmitted from one person to another through tattooing? (2013)
- Chikungunya
- Hepatitis B
- HIV-AIDS
Select the correct answer using the codes given below:
(a) 1 only
(b) 2 and 3 only
(c) 1 and 3 only
(d) 1, 2 and 3
Ans: (b)
Mains
Q. Can overuse and free availability of antibiotics without a doctor’s prescription contribute to the emergence of drug-resistant diseases in India? What are the available mechanisms for monitoring and control? Critically discuss the various issues involved.(2014)

.png)