Governance
Reforming the Euthanasia Framework in India
This editorial is based on “Reforming passive euthanasia in India”, which was published in The Hindu on 07/10/2025. The article explains that the UK has passed a bill allowing terminally ill adults to choose assisted dying under strict safeguards, while India, facing cultural and systemic challenges, continues to permit only passive euthanasia and should focus on making its existing laws more practical and humane.
For Prelims: Euthanasia, Aruna Shanbaug v. Union of India (2011), Common Cause v. Union of India (2018), Right to die with dignity
For Mains: Key Arguments Supporting the Legalisation of Euthanasia, Major Concerns that Argue Against the Legalisation of Euthanasia
The UK’s Terminally Ill Adults (End of Life) Bill, recently passed by the House of Commons, would legalise assisted dying for terminally ill adults with less than six months to live, subject to strict safeguards and multiple medical approvals. This legislation aims to provide dying individuals choice and dignity while ensuring protection against coercion. It contrasts with India’s cautious approach, which limits euthanasia to passive forms and faces challenges of accessibility and ethical complexities.
What is Euthanasia?
- About: Euthanasia, derived from the Greek words ‘eu’ (good) and ‘thanatos’ (death), means "good death" or the intentional act of ending a life to relieve unbearable suffering caused by incurable or terminal illness.
- It often refers to a painless, deliberate intervention to end life with the primary aim of alleviating physical, emotional, or spiritual distress.
- Types: Euthanasia is broadly classified into the following types based on consent and method.
- Based on consent :
- Voluntary Euthanasia: Performed with the informed consent of a mentally competent patient who requests to end their life.
- Non-voluntary Euthanasia: Conducted when the patient is unable to give consent (e.g., unconscious or mentally incapacitated), and a surrogate decision-maker authorises it.
- Involuntary Euthanasia: Done against the patient's will or without asking, considered illegal and ethically unacceptable.
- Based on method:
- Active Euthanasia: Direct action to cause death, such as administering a lethal injection.
- Passive Euthanasia: Withholding or withdrawing life-sustaining treatment, allowing death to occur naturally.
- Based on consent :
- Legal Aspects Globally:
- Countries like the Netherlands, Belgium, Canada, and some U.S. states legally permit voluntary active euthanasia or physician-assisted suicide under strict safeguards.
- In most countries, active euthanasia remains illegal and may be considered homicide.
- Assisted suicide differs as the patient self-administers lethal medication, while euthanasia involves a third party causing death.
- Legal Status in India:
- Active Euthanasia: Deliberately causing death through acts like administering lethal substances was considered illegal and punishable under the Indian Penal Code (IPC).
- The newer BNS continues this stance, criminalising active euthanasia to prevent misuse and protect life.
- Sections 100 and 101 of the Bharatiya Nyaya Sanhita (BNS) define culpable homicide and murder, meaning that any act of killing, including euthanasia, is considered a crime unless it falls under certain legal exceptions.
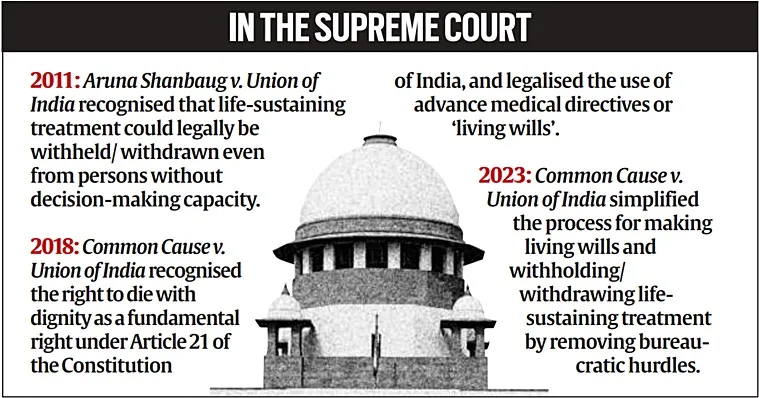
- Passive Euthanasia: Legally permitted since the landmark Supreme Court judgment in Aruna Shanbaug v. Union of India (2011) and further clarified in Common Cause v. Union of India (2018), passive euthanasia involves withholding or withdrawing life-supporting treatment, allowing natural death.
- Active Euthanasia: Deliberately causing death through acts like administering lethal substances was considered illegal and punishable under the Indian Penal Code (IPC).
What are the Key Arguments Supporting the Legalisation of Euthanasia?
- Respect for Patient Autonomy: Legalising euthanasia affirms an individual's right to make decisions about their own body and life, including the right to choose a dignified death when facing unbearable suffering.
- This aligns with modern views on personal freedoms and self-determination.
- The Supreme Court of India’s 2018 ruling in Common Cause vs Union of India recognised the “right to die with dignity” under Article 21, allowing patients to create advance medical directives or living wills.
- Relief from Suffering: Many patients with terminal illnesses endure intense physical or psychological pain that cannot be fully alleviated by palliative care.
- Euthanasia offers a compassionate choice to end such suffering humanely.
- For example, over 60% of euthanasia deaths in countries where it is legal relate to cancer patients experiencing severe pain.
- Reduction of Prolonged and Futile Treatment: Euthanasia can prevent unnecessary medical interventions that prolong suffering without reasonable hope of recovery, reducing emotional and financial burdens on families and healthcare systems.
- Passive euthanasia is legally permitted in India under strict guidelines (such as in the Aruna Shanbaug case, 2011), enabling withdrawal of futile treatment.
- Improved Quality of End-of-Life Care: Legalisation encourages better hospice and palliative care frameworks by bringing euthanasia into regulated medical practice, emphasising patient comfort and dignity.
- In India, where palliative care access remains limited, euthanasia can provide a compassionate option to end prolonged suffering.
- Global Practices as a Reference: Nations such as the Netherlands, Belgium, and Canada have established comprehensive legal frameworks for euthanasia that incorporate strict safeguards, multi-tier medical oversight, and consent verification mechanisms.
- India can draw lessons from these models to design a balanced approach that upholds patient autonomy while preventing misuse.
What are the Major Concerns that Argue Against the Legalisation of Euthanasia?
- Ethical and Moral Opposition: Many in Indian society view euthanasia as morally wrong, believing in the sanctity of life as inviolable.
- Religious and cultural beliefs strongly oppose active ending of life, considering it equivalent to murder.
- Risk of Abuse and Coercion: Vulnerable groups such as the elderly, disabled, and financially dependent are at risk of being pressured or coerced into choosing euthanasia.
- In India, where socioeconomic disparities and uneven healthcare access exist, families or caregivers may influence decisions for financial, emotional, or practical reasons, compromising the patient’s true autonomy.
- Such coercion could lead to unethical practices and undermine the principle of voluntary choice.
- Difficulty in Assessing Mental Capacity: Psychiatric assessments are essential to ensure that patients requesting euthanasia are mentally competent and are making informed decisions.
- However, many psychiatrists in India report lacking confidence in diagnosing depression or detecting subtle coercion, especially in terminally ill patients.
- This increases the likelihood of inappropriate euthanasia approvals, potentially resulting in ethical and legal complications for medical professionals.
- Legal Ambiguities and Criminalisation:Under the Indian Penal Code, active euthanasia and assisted suicide are considered criminal acts.
- Acts amounting to active euthanasia or assisted suicide can be prosecuted under the Bharatiya Nyaya Sanhita (BNS), 2023 .
- Sections 100 and 101 of the BNS define culpable homicide and murder, rendering any act of killing, including euthanasia, a criminal offence unless it falls under specified exceptions. Additionally, Section 108 criminalises abetment of suicide, further complicating the legal framework surrounding active euthanasia.
- The legal framework lacks clear legislation to regulate euthanasia, generating ambiguity and risk for practitioners.
- Procedural Complexity and Judicial Burden: Even passive euthanasia requires court approval and multiple medical boards per Supreme Court guidelines, rendering the process slow and inaccessible for many families, thereby limiting practical application.
- Public Awareness and Attitude Variability: Studies from regions like Kerala indicate varied public knowledge and mixed attitudes toward euthanasia, with less than 40% supporting ending life voluntarily.
- This gap complicates policy acceptance.
- Concerns Over Impact on Palliative Care: Critics argue that legalising euthanasia might reduce efforts and resources devoted to palliative care, which remains underdeveloped in India.
- Medical professionals emphasise improving pain management over ending life.
- According to the World Health Organisation (WHO), over 40 million people worldwide require palliative care annually, yet only 14% actually receive it.
- In India, an estimated 7 to 10 million people need palliative support each year, but access remains extremely limited, reaching barely 4% of those in need, highlighting significant healthcare gaps and the urgent need to strengthen palliative infrastructure.
What Measures Can India Adopt to Ensure Dignified End-of-Life Care?
- Streamline Passive Euthanasia Procedures: In January 2023, the Supreme Court of India simplified the process for passive euthanasia by removing the mandatory requirement of judicial magistrate attestation for advance medical directives (living wills), allowing notarization or gazetted officer attestation instead.
- Integrating living wills into the National Health Digital Record ensures easy access by medical professionals nationwide, expediting decision-making.
- Develop a Clear Legislative Framework: The Supreme Court has laid down guidelines but emphasised Parliament should enact comprehensive legislation, especially to clearly distinguish active and passive euthanasia and regulate advance directives.
- A robust law will reduce ambiguity, protect medical practitioners from legal risks, and provide procedural clarity.
- Institutionalise Hospice and Palliative Care: Expanding and strengthening palliative care infrastructure is critical, as current access in India is much less than that of those in need.
- International models (e.g., Holland’s palliative networks) highlight how palliative care reduces demand for euthanasia by alleviating pain effectively.
- Create Multidisciplinary Hospital Ethics Committees: Hospitals should establish ethics committees comprising doctors, legal experts, and social workers to oversee euthanasia decisions, ensuring patient consent, mental capacity checks, and ethical compliance.
- This decentralises oversight and reduces delays caused by court involvement.
- Train Medical and Legal Professionals: Specialised training programs on end-of-life care, legal aspects of euthanasia, and psychiatric evaluation can improve the diagnosis of patient capacity and ethical decision-making.
- This reduces misuse risks stemming from improper assessments.
- Enhance Public Awareness and Education: Promote awareness campaigns about living wills, end-of-life choices, and euthanasia’s legal status to encourage informed patient decisions and family support.
- Incorporate cooling-off periods, mandatory psychological counselling, and review by independent medical boards to prevent coercion and wrongful euthanasia.
Conclusion:
The debate on euthanasia in India balances individual autonomy with ethical, cultural, and legal values. Supreme Court rulings recognise the right to die with dignity via passive euthanasia and advance directives, yet procedural complexity, societal diversity, and healthcare disparities remain challenges. As Mahatma Gandhi noted, “ The true measure of any society can be found in how it treats its most vulnerable members.” Strengthening laws, palliative care, and public education provides a compassionate, regulated path forward.
|
Drishti Mains Question : Analyse the arguments for and against the legalisation of active euthanasia in India within the constitutional mandate of the right to life. |
Frequently Asked Questions (FAQs)
1. What does the UK’s Terminally Ill Adults (End of Life) Bill propose?
Ans: The Bill legalises assisted dying for terminally ill adults with less than six months to live, under strict safeguards and medical oversight, aiming to ensure choice and dignity while preventing coercion.
2. What is the current legal status of euthanasia in India?
India allows passive euthanasia under Supreme Court judgments — Aruna Shanbaug (2011) and Common Cause (2018) — recognising the right to die with dignity under Article 21, while active euthanasia remains illegal under Sections 302 and 305 IPC.
3. What are the key challenges to euthanasia legalisation in India?
Major issues include ethical opposition, risk of coercion, mental capacity assessment difficulties, legal ambiguities, and low public awareness, along with poor palliative care access (only 4% coverage despite 7–10 million needing it annually).
4. What measures has the Supreme Court taken to simplify passive euthanasia procedures?
In January 2023, the Supreme Court removed judicial magistrate attestation for living wills, allowing notarization or gazetted officer approval, and recommended integrating them into the National Health Digital Record for quicker access.
5. What practical steps can India take to ensure dignified end-of-life care?
India should enact a comprehensive euthanasia law, expand palliative and hospice care, create hospital ethics committees, train medical professionals, and raise public awareness to ensure ethical, accessible, and compassionate end-of-life care.
UPSC Civil Services Examination, Previous Year Questions (PYQs)
Prelims
Q. Right to Privacy is protected as an intrinsic part of Right to Life and Personal Liberty. Which of the following in the Constitution of India correctly and appropriately imply the above statement? (2018)
(a) Article 14 and the provisions under the 42nd Amendment to the Constitution.
(b) Article 17 and the Directive Principles of State Policy in Part IV.
(c) Article 21 and the freedoms guaranteed in Part III.
(d) Article 24 and the provisions under the 44th Amendment to the Constitution.
Ans: (C)
Mains
Q. In order to enhance the prospects of social development, sound and adequate health care policies are needed particularly in the fields of geriatric and maternal health care.Discuss.(2020)