Governance
India's Road to Universal Health Coverage
- 02 Jun 2025
- 16 min read
This editorial is based on “The road to Universal Health Coverage in India” which was published in The Indian Express on 30/05/2025. The article brings into picture the push for Universal Health Coverage through Ayushman Bharat, highlighting gaps like 400 million uninsured, and stresses the need to balance booming private healthcare with stronger public investment in primary care.
For Prelims: Ayushman Bharat, Ayushman Arogya Mandir, Ayushman Bharat Digital Mission, National Tele Mental Health Programme , 2023 Medical Device Policy,Non-communicable diseases, Zoonotic diseases.
For Mains: Key Recent Developments in India's Healthcare Sector, Key Issues Hindering the Effectiveness of India's Healthcare Sector
India stands at a critical juncture in its healthcare journey, with the Ayushman Bharat initiative targeting Universal Health Coverage by 2030 while the private healthcare sector rapidly expands to an estimated $610 billion by 2026. Despite progress in reducing out-of-pocket expenses from 60-70% to 39.4%, nearly 400 million Indians still lack health insurance coverage, particularly affecting outpatient care which accounts for two-thirds of healthcare spending. The path forward requires balancing private sector growth with strengthened public investment in preventive and primary care to ensure healthcare access based on need rather than purchasing power.
What are the Key Recent Developments in India's Healthcare Sector?
- Expansion through Ayushman Arogya Mandirs: Strengthening primary health care is crucial for universal health coverage and reducing the burden on tertiary facilities.
- The Ayushman Bharat initiative’s transformation of more than 1.7 lakh Health and Wellness Centres by March 2024 exemplifies this focus.
- These centres integrate preventive, promotive, and rehabilitative care, including Yoga and AYUSH, addressing holistic health needs.
- The AAMs grew at a CAGR of 46.6% from 2018-19 to 2023-24.
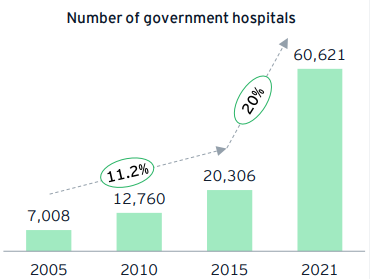
- Surge in Public Hospitals Growth: Robust healthcare delivery depends on infrastructure availability; hence, increasing public hospitals improves accessibility and affordability.
- From 7,008 hospitals in 2005 to 60,621 in 2021, India recorded a CAGR of 14.4% in public hospitals, reflecting massive infrastructure scaling.
- This expansion alleviates strain on urban hospitals and improves rural healthcare reach, vital for equitable health outcomes.
- Digital Transformation in Healthcare Delivery: Digital tools are revolutionizing healthcare access, improving efficiency, transparency, and data-driven decision making.
- Initiatives like the Ayushman Bharat Digital Mission, CoWIN, Aarogya Setu, and e-Sanjeevani have digitally connected millions, enhancing telemedicine and pandemic response.
- Over 2.96 lakh health professionals are registered on the Health Professionals Registry (HPR), enabling interoperable digital services nationwide.
- Expanding Health Insurance Coverage via PM-JAY: Reducing catastrophic out-of-pocket expenses requires robust health insurance coverage and financial risk protection.
- PM-JAY extends coverage to nearly 15 crore families, with INR 5 lakh per family annually, encompassing secondary and tertiary care with 1,900 packages and no pre-existing condition exclusions.
- So far, 6.5 crore hospital admissions worth INR 81,979 crore have been authorized, demonstrating scale and impact.
- Enhanced Focus on Disease Surveillance and Prevention: Early detection and prevention of communicable diseases remain key to reducing health system burden.
- The Integrated Disease Surveillance Programme (IDSP), operational since 2004, strengthens public health monitoring for rapid outbreak response.
- Combined with Janani Suraksha schemes, these programs significantly contribute to reducing morbidity and mortality.
- Increase in Public Healthcare Utilization and Quality Standards: Rising trust in public healthcare is visible as government hospitals’ share of OPD and IPD rose by over 25% since 2014, reflecting improved access and affordability.
- Implementation of National Quality Assurance Standards (NQAS) for hospitals and PHCs ensures benchmarked service quality, promoting patient safety and satisfaction nationwide.
- Growing Pharmaceutical Industry and Medical Device Sector: India’s pharma sector, the “pharmacy of the world,” is expanding with a projected market size of $130 billion by 2030, boosting affordable access and exports.
- The 2023 Medical Device Policy enhances domestic manufacturing capacity and quality, aligning with Make in India and Atma Nirbhar Bharat initiatives to reduce import dependence and foster innovation.
- Strengthened Healthcare Workforce and Education: An adequate, skilled workforce is the backbone of quality healthcare; hence, India has ramped up medical and nursing education.
- Registered nurses increased from 14.81 lakh in 2005 to 36.14 lakh in 2022 (CAGR ~4.9%), while allopathic doctors rose from 6.6 lakh to 13.08 lakh (CAGR ~4.1%).
- The FY23 budget’s 157 new nursing colleges will address workforce shortages and global demand for Indian nurses.
What are the Key Issues Hindering the Effectiveness of India's Healthcare Sector?
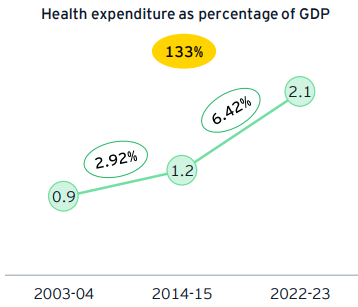
- Inadequate Public Health Expenditure: Low and uneven public spending constraints infrastructure, workforce, and quality improvements in healthcare.
- India’s public health expenditure is just 2.1% of GDP (2022-23), below the recommended 2.5% by the 15th Finance Commission.
- This limits the scaling up of critical services despite growing demand. Many developed countries allocate 5-10% of GDP to health, underscoring India’s underinvestment challenge.
- Persistently High Out-of-Pocket Expenditure (OOPE): High OOPE leads to financial hardship and pushes millions into poverty, limiting healthcare access for vulnerable populations.
- Despite progress, OOPE remains at 39.4%, with outpatient care accounting for two-thirds of this spending.
- Drugs alone constitute over 67% of OOPE, emphasizing the need for affordable medicines and insurance coverage expansion.
- Absence of uniform standards and unchecked commercialization result in variable quality and high costs.
- Insufficient Insurance Coverage and Focus on Outpatient Care: Nearly 400 million Indians remain uninsured, especially for outpatient expenses which dominate healthcare costs.
- PM-JAY mainly covers inpatient hospitalization, leaving outpatient and chronic care uncovered, impacting affordability and early intervention.
- The gap in comprehensive coverage hampers Universal Health Coverage goals by 2030.
- Skewed Healthcare Workforce Distribution and Shortages: Though numbers of doctors and nurses have risen, there is a significant urban-rural and public-private imbalance affecting access and quality.
- Though India's doctor-population ratio at 1:854 is better than the World Health Organisation's standard of 1:1000, rural areas face acute shortages, and registered AYUSH practitioners remain underutilized despite growing demand for integrative medicine.
- Also, private facilities cater largely to urban and affluent populations, creating disparities.
- Though India's doctor-population ratio at 1:854 is better than the World Health Organisation's standard of 1:1000, rural areas face acute shortages, and registered AYUSH practitioners remain underutilized despite growing demand for integrative medicine.
- Infrastructure Deficits and Quality Gaps in Public Facilities: Though public hospitals have expanded, many still suffer from inadequate beds, equipment, and maintenance, affecting patient outcomes.
- India’s hospital bed density remains around 0.5 beds per 1,000 population, well below WHO’s 3 beds per 1,000 benchmark.
- Quality gaps persist despite National Quality Assurance Standards (NQAS), especially in rural and remote areas.
- Limited Emphasis on Preventive and Primary Care: Healthcare remains skewed towards curative tertiary care rather than prevention and primary health services.
- Non-communicable diseases (NCDs) now account for over 60% of deaths, yet preventive outreach is insufficient.
- Strengthening Health and Wellness Centres is ongoing but needs faster scaling and integration with community health workers.
- Data Privacy Issues in Digital Health Integration: While digital health initiatives have progressed, interoperability, data privacy, and inclusion remain issues.
- For instance, the Indian healthcare industry faced more than 1.9 million cyberattacks in 2022. Major cyber attacks reported around India over the past five years involved hospitals, including AIIMS Delhi and Safdarjung Hospital.
What Measures can India Adopt to Enhance the Healthcare Sector?
- Strengthen and Integrate Primary Healthcare Networks: Transform Ayushman Arogya Mandirs into vibrant hubs that not only deliver comprehensive primary care but also synergize with sanitation (Swachh Bharat), nutrition (Poshan Abhiyan), and education initiatives.
- This integrated model will enhance health determinants holistically, promote early disease detection, and significantly reduce the tertiary care burden.
- Creating robust referral linkages and ensuring seamless data flow across PHCs, CHCs, and higher centers can institutionalize continuity of care and equity in access.
- Revolutionize Health Workforce Capacity: Adopt an incentive-driven ecosystem incorporating rural service bonds, accelerated career progression, and financial rewards to retain healthcare professionals in underserved areas.
- Align medical education curricula with community health needs and embed training for multidisciplinary health workers, including AYUSH practitioners, through schemes like the National Health Mission.
- This will create a resilient, versatile workforce attuned to India’s epidemiological transition and demographic diversity.
- Expand Universal Health Insurance to Holistically Cover Outpatient, Preventive, and Chronic Care: India can rethink PM-JAY and insurance schemes to encompass outpatient diagnostics, medicines, and preventive screenings, tackling the major share of out-of-pocket expenditure (only to most vulnerable section in initial stages).
- Introduce modular insurance products for chronic diseases management, incentivizing early intervention and reducing hospitalization.
- This paradigm shift will ensure financial risk protection while aligning with global best practices for universal health coverage.
- Unified Regulatory Framework for Private Healthcare with Digital Oversight: Create a centralized regulatory authority empowered to enforce comprehensive quality standards, ethical pricing, and grievance redressal across private providers.
- Integrate this framework with digital health initiatives such as ABDM and hospital accreditation bodies to enable real-time monitoring and transparency.
- Such harmonization will foster trust, reduce exploitative practices, and promote equitable healthcare delivery.
- Driving Data-Enabled, Patient-Centric Care: Accelerate the nationwide implementation of interoperable digital health records linked to AI-powered analytics for predictive disease modeling, resource optimization, and personalized care pathways.
- Ensure 100% registration of healthcare professionals and facilities on the Health Professionals Registry and Healthcare Facilities Registry under ABDM.
- Concurrently, enforce stringent data privacy and cybersecurity frameworks to build citizen confidence and promote ethical data use.
- Drive Innovation and Self-Reliance in Pharmaceuticals and Medical Devices: Promote public-private partnerships and increase R&D funding for frontier technologies like organ bioprinting, robotics, and AI diagnostics under the Medical Device Policy 2023.
- Facilitate backward integration in supply chains and streamline regulatory approvals to bolster India’s global competitiveness.
- Align these initiatives with the Make in India and Aatmanirbhar Bharat missions to transform India into a global hub for affordable, high-quality healthcare innovation.
What India can Learn from Others in Healthcare?
- Universal Primary Care Access: Adopt Brazil’s Family Health Strategy for community-based primary care coverage.
- Efficient Health Financing: Learn from Thailand’s Universal Coverage Scheme to reduce out-of-pocket expenses.
- Digital Health Integration: Emulate Estonia’s nationwide e-health record system for seamless data sharing.
- Public-Private Collaboration: Study Germany’s regulated private insurance and public system synergy.
- Preventive Health Focus: Incorporate Finland’s successful non-communicable disease prevention programs (North Karelia Project).
Conclusion:
India’s healthcare transformation demonstrates significant progress toward achieving Universal Health Coverage, aligning with Sustainable Development Goal 3 (Good Health and Well-being). To move from reactive to preventive care, India must balance the rapid growth of its private healthcare sector with increased public investment in primary health systems, digital integration, and health workforce expansion. A people-centric, inclusive, and resilient healthcare ecosystem is essential to ensure equitable access and financial protection for all by 2030.
|
Drishti Mains Question: “India’s healthcare system is witnessing rapid digitalization and private sector expansion, yet equitable access and financial protection remain elusive for millions.” Discuss. |
UPSC Civil Services Examination, Previous Year Questions (PYQs)
Prelims
Q. Which of the following are the objectives of ‘National Nutrition Mission’? (2017)
- To create awareness relating to malnutrition among pregnant women and lactating mothers.
- To reduce the incidence of anaemia among young children, adolescent girls and women.
- To promote the consumption of millets, coarse cereals and unpolished rice.
- To promote the consumption of poultry eggs.
Select the correct answer using the code given below:
(a) 1 and 2 only
(b) 1, 2 and 3 only
(c) 1, 2 and 4 only
(d) 3 and 4 only
Ans: (a)
Mains
Q. “Besides being a moral imperative of a Welfare State, primary health structure is a necessary precondition for sustainable development.” Analyse. (2021)