Social Justice
India’s Path to Global Health Leadership
- 02 May 2025
- 15 min read
This editorial is based on “ Landmark agreement: On the draft WHO Pandemic Agreement” which was published in The Hindu on 22/04/2025. The article brings into picture the finalized WHO Pandemic Agreement, which ensures fair pathogen sharing and access to treatments.
For Prelims: WHO Pandemic Agreement, Non-communicable diseases, Antimicrobial resistance, Climate change, Monkeypox,International Health Regulations (IHR) 2005, Non-Communicable Diseases, CoWIN , Ayushman Bharat Digital Mission
For Mains: Key Health Challenges Confronting the Globe, Current Institutional Framework Governing Global Health Management.
The recent finalization of the proposal of WHO Pandemic Agreement marks a watershed moment in global health governance. While more limited than initially envisioned, the agreement establishes crucial pathogen sharing and benefit systems that guarantee developing nations access to treatments derived from their shared samples. India, with its robust pharmaceutical industry, diplomatic influence as a voice for the Global South, and experience navigating health crises, is uniquely positioned to play a pivotal role in implementing this agreement and shaping more equitable global health architectures.
What are the Key Health Challenges Confronting the Globe?
- Inequitable Access to Vaccines and Medical Countermeasures: A significant global health issue remains the unequal distribution of vaccines, diagnostics, and treatments, particularly between developed and developing countries.
- Despite global efforts, many low- and middle-income countries (LMICs) still face delays in accessing essential health products.
- During the Covid-19 pandemic, over 80% of the vaccines were administered in high-income countries (2021), while LMICs struggled with access.
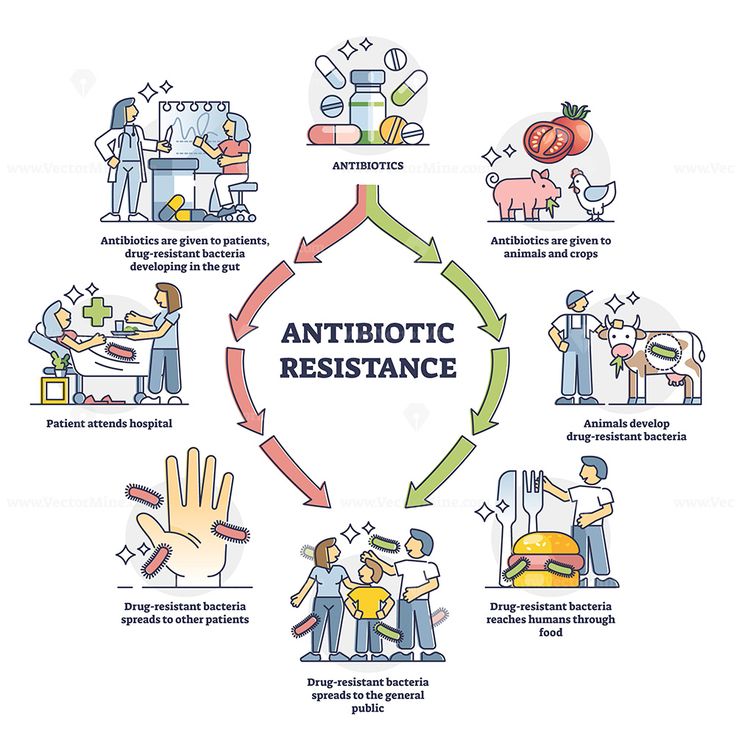
- Growing Threat of Antimicrobial Resistance: Antimicrobial resistance (AMR) is rapidly becoming one of the most pressing global health threats, exacerbated by overuse and misuse of antibiotics.
- AMR leads to the development of "superbugs" that cannot be treated by standard antibiotics, threatening the effectiveness of medical treatments globally.
- By 2030, antimicrobial resistance could force up to 24 million people into extreme poverty. Currently, at least 700,000 people die each year due to drug-resistant diseases
- Non-Communicable Diseases and Lifestyle-Related Health Risks: Non-communicable diseases (NCDs) like heart disease, diabetes, and cancer continue to rise globally, fueled by lifestyle factors such as poor diet, lack of physical activity, and tobacco use.
- These diseases place a massive burden on global health systems, particularly in low- and middle-income countries that lack sufficient healthcare infrastructure to address prevention and treatment.
- According to WHO, NCDs account for 71% of global deaths annually, with the majority of these deaths occurring in low- and middle-income countries.
- The Covid-19 pandemic further exacerbated NCDs as lifestyle disruptions led to an increase in mental health issues and unhealthy habits globally.
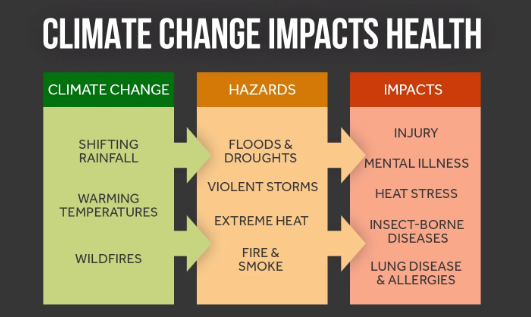
- Climate Change and its Impact on Health: Climate change is increasingly recognized as a major global health threat, with rising temperatures, extreme weather events, and environmental degradation affecting human health.
- The direct effects include respiratory diseases due to pollution and heat-related illnesses, while the indirect effects exacerbate food insecurity, water scarcity, and the spread of infectious diseases.
- Research shows that 3.6 billion people already live in areas highly susceptible to climate change.
- Between 2030 and 2050, climate change is expected to cause approximately 250 000 additional deaths per year, from undernutrition, malaria, diarrhoea and heat stress alone.
- Mental Health Crisis: The mental health crisis has escalated, worsened by the social and economic effects of the COVID-19 pandemic.
- The global rise in mental health disorders, including depression and anxiety, has put a strain on healthcare systems worldwide, demanding more attention to mental health care as part of public health strategies.
- For instance, the WHO reported a 25% increase in anxiety and depression worldwide during the first year of the Covid-19 pandemic.
- In India, national studies reveal that 15% of India’s adult population experiences mental health issues requiring intervention. Urban areas have a higher prevalence (13.5%) compared to rural (6.9%).
- Health Workforce Shortages and Migration: A shortage of trained healthcare professionals is a major challenge in many parts of the world, especially in rural and underserved regions.
- The migration of healthcare workers from low-income to high-income countries exacerbates this issue, highlighting the need for better workforce training, retention strategies, and international cooperation on healthcare labor policies.
- A recent research estimated that in 2020, the global workforce stock was 29.1 million nurses, 12.7 million medical doctors, 3.7 million pharmacists.
- Rise of Infectious Diseases and Emerging Pathogens: Emerging infectious diseases, such as the recent outbreak of Monkeypox and the continued threat of diseases like Ebola and Zika, underscore the vulnerability of the global health system.
- Preparedness, rapid response, and international collaboration are crucial to preventing the spread of these diseases, which can have global implications.
- For instance, the World Health Organization declared Monkeypox a Public Health Emergency of International Concern (PHEIC) in 2022.
- Similarly, the resurgence of Ebola in West Africa in 2021 highlighted the need for stronger global surveillance and containment systems.
What is the Current Institutional Framework Governing Global Health Management?
- World Health Organization (WHO) Framework: The World Health Organization (WHO) is the cornerstone of global health management, guiding international health policies and providing leadership in coordinating health responses.
- WHO’s key functions include setting international health standards, offering technical support to countries, and overseeing the implementation of health protocols.
- Global Health Security Agenda (GHSA): The GHSA is a global initiative (India is a member) aimed at strengthening countries' capacities to prevent, detect, and respond to infectious disease threats.
- The agenda focuses on improving national health systems, surveillance, and emergency response mechanisms to safeguard against pandemics.
- International Health Regulations (IHR) 2005: The International Health Regulations (IHR), governed by WHO, are a legally binding framework aimed at ensuring the global health response to public health emergencies is swift and coordinated.
- IHR facilitates the exchange of information regarding infectious disease outbreaks and sets the standard for countries’ preparedness and responses to public health risks.
- Global Fund to Fight AIDS, Tuberculosis, and Malaria: The Global Fund is a global financing initiative designed to combat the three major infectious diseases: AIDS, tuberculosis, and malaria.
- The Fund partners with countries to strengthen health systems, promote disease prevention, and support treatment programs.
- GAVI - The Vaccine Alliance: GAVI, or the Global Alliance for Vaccines and Immunization, is a public-private partnership aimed at increasing access to immunization in low-income countries.
- Its mission is to provide life-saving vaccines to the most vulnerable populations, reducing disparities in vaccine access across the globe.
- GAVI works with governments, the World Health Organization (WHO), UNICEF, the World Bank, and other partners to improve immunization rates, particularly in low-resource settings.
What Role can India Assume in Shaping and Advancing Global Health Governance?
- Leadership in Pandemic Preparedness and Response: India can play a crucial role in leading global health governance by strengthening pandemic preparedness and response mechanisms.
- As the Covid-19 pandemic highlighted gaps in global coordination, India’s advocacy for a robust and coordinated response, through its leadership in the G20 and SCO, positions it as a key player in shaping international health strategies.
- Strengthening WHO and Global Health Diplomacy: India has emerged as a prominent advocate for a more inclusive and reformed WHO, underscoring the need for an agile, responsive health governance framework.
- The country’s support for the WHO’s Pandemic Treaty and its efforts to reform international health regulations highlight India’s commitment to a multilateral, cooperative approach.
- India’s nine-point reform proposal for the WHO, post-COVID-19, emphasized the importance of enhancing global health governance processes.
- Promoting Equitable Access to Medicines and Vaccines: India’s pharmaceutical prowess positions it as a cornerstone in ensuring global access to affordable medicines.
- By leveraging its robust generics sector, India has facilitated the global supply of life-saving medications, including vaccines, especially during the Covid-19 pandemic.
- India also accounts for 60 per cent of global vaccine production making it the largest vaccine producer in the world.
- The Serum Institute’s production of the Oxford-AstraZeneca vaccine was pivotal in making vaccines available to low- and middle-income countries, especially in Africa and Asia.
- Integration of Traditional and Modern Medicine in Global Health: India can bridge the gap between traditional and modern medicine, offering a holistic approach to health governance.
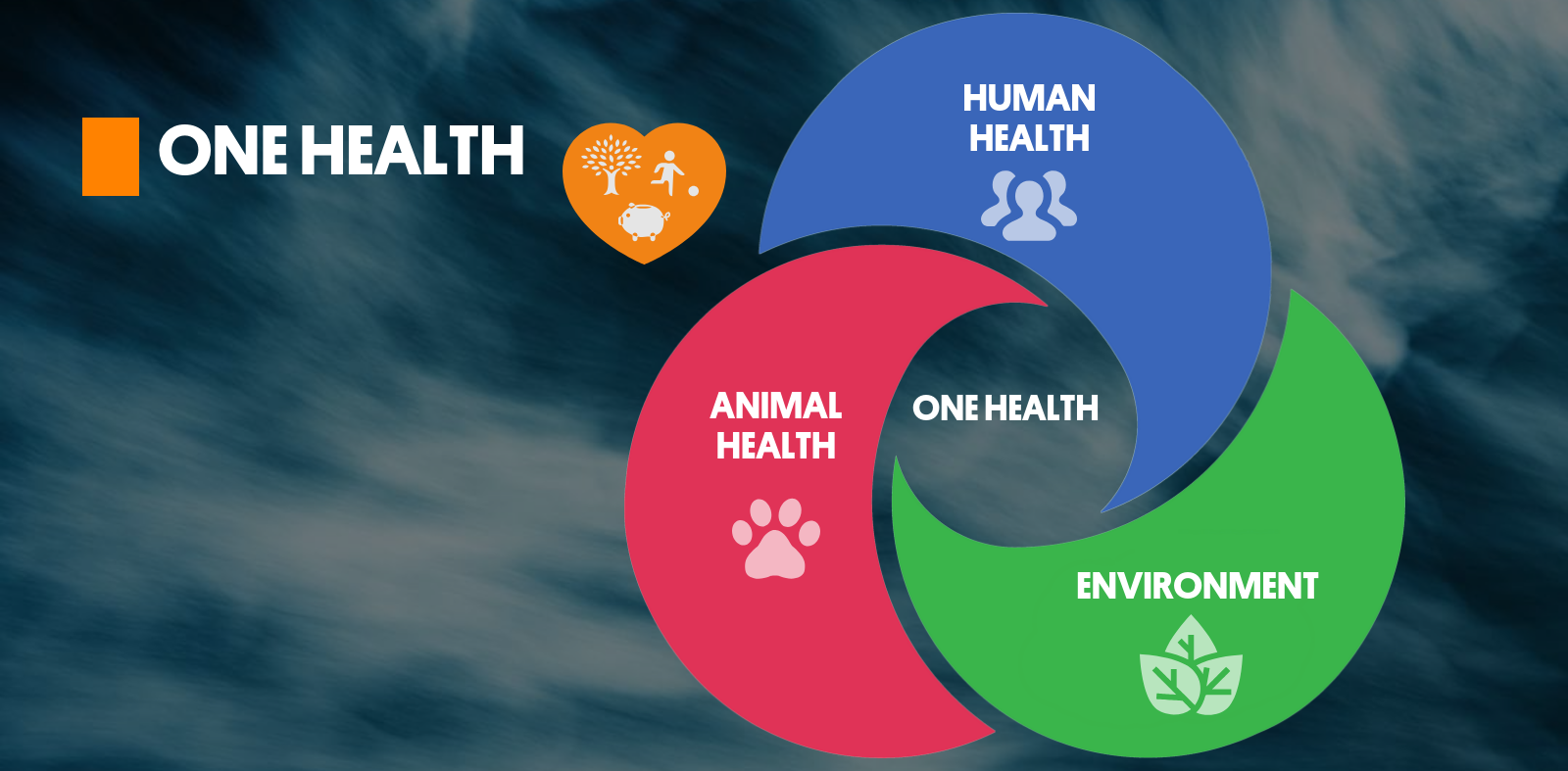
- With its rich heritage in Ayurveda, Yoga, and other traditional practices, India has promoted the concept of "One Health"—recognizing the interconnectedness of human, animal, and environmental health.
- This integration is particularly relevant in addressing non-communicable diseases (NCDs) and emerging health issues.
- The AYUSH guidelines, along with traditional remedies for diseases like filariasis, underscore India's contribution to global health practices.
- With its rich heritage in Ayurveda, Yoga, and other traditional practices, India has promoted the concept of "One Health"—recognizing the interconnectedness of human, animal, and environmental health.
- Facilitating Digital Health and Health Technology: India’s advancements in digital health infrastructure, particularly through initiatives like the Ayushman Bharat Digital Mission, provide a framework for global health innovation.
- By sharing its e-health solutions globally, India can help other nations improve their health information exchange and telemedicine capabilities.
- This integration of digital health into public policy makes India a leader in tech-enabled health governance.
- India offered CoWIN as a "digital public good" to the world, asserting that it is committed to sharing its digital health expertise.
- By sharing its e-health solutions globally, India can help other nations improve their health information exchange and telemedicine capabilities.
- Expanding Health Cooperation through Global South Engagement: India’s role in the Global South enhances its capacity to shape global health governance by promoting South-South cooperation.
- India fosters stronger diplomatic ties and positions itself as a champion of equitable health solutions.
- India’s Vaccine Maitri initiative provided millions of vaccine doses to South Asian and African countries, strengthening India’s influence in these regions.
Conclusion
Despite persistent challenges like inequity, AMR, and workforce gaps, the globe is finding ends to reshape health governance. India, with its (Pharma Shakti) pharmaceutical strength, traditional wisdom (Ayurveda), and digital innovation, can emerge as a Vishwa Mitra in building an inclusive, resilient, and just global health order. As the world reimagines health governance, India's role must be both strategic and compassionate.
|
Drishti Mains Question: In the backdrop of evolving global health challenges and the recent WHO Pandemic Agreement, critically examine India’s role in shaping global health governance. |
UPSC Civil Services Examination Previous Year Question (PYQ)
Prelims
Q. Which of the following are the objectives of ‘National Nutrition Mission’? (2017)
- To create awareness relating to malnutrition among pregnant women and lactating mothers.
- To reduce the incidence of anaemia among young children, adolescent girls and women.
- To promote the consumption of millets, coarse cereals and unpolished rice.
- To promote the consumption of poultry eggs.
Select the correct answer using the code given below:
(a) 1 and 2 only
(b) 1, 2 and 3 only
(c) 1, 2 and 4 only
(d) 3 and 4 only
Ans: (a)
Mains
Q. “Besides being a moral imperative of a Welfare State, primary health structure is a necessary precondition for sustainable development.” Analyse. (2021)
Q. Appropriate local community-level healthcare intervention is a prerequisite to achieve ‘Health for All’ in India. Explain. (2018)