Social Justice
Shorter Medical Course to Address Rural Doctor Shortage
- 26 Jun 2023
- 8 min read
For Prelims: Ayushman Bharat, National Health Mission, Accredited Social Health Activists
For Mains: Potential of India’s Healthcare Sector, Issues Associated with India’s Healthcare Sector, Recent Government Initiatives Related to Healthcare.
Why in News?
Recently, the West Bengal Chief Minister proposed a Shorter Medical Course for medical practitioners who would serve in primary health centers (PHCs) in rural areas.
- This proposal aims to address the chronic shortage of doctors in rural regions where a significant percentage (around 65%) of the Indian population resides.
- Similar initiatives have been implemented in other states, such as Chhattisgarh, which introduced a three-year community health program producing Rural Medical Assistants (RMAs) to serve in villages.
What is the Proposed Shorter Medical Course for Rural Areas?
- About:
- A shorter medical course proposed in India is a three-year diploma course for medical practitioners who would serve in primary health centres (PHCs) in rural areas. This course is different from the regular MBBS course.
- The shorter medical course focuses on providing first-level care in rural areas, while the regular MBBS course covers all aspects of medical science and practice.
- The shorter medical course may not train trainees adequately to deal with complex and diverse conditions in rural areas, while the regular MBBS course prepares doctors for any kind of situation.
- Benefits:
- Increased availability of medical professionals in rural areas.
- Rapid response to healthcare needs and emergencies.
- Cost-effective solution for resource-constrained regions.
- Enhanced primary healthcare services in rural communities.
- Drawbacks:
- Limited specialization in complex medical fields.
- Insufficient exposure to rural healthcare conditions.
- Potential dilution of medical education standards.
- It will raise concerns about potential discrimination, as it could result in less qualified healthcare providers being assigned to rural populations while urban settings receive more qualified practitioners.
- Does not address underlying structural issues contributing to the shortage of doctors.
What is the Status of Doctors in Rural India as per Rural Health Statistics Report 2021-22?
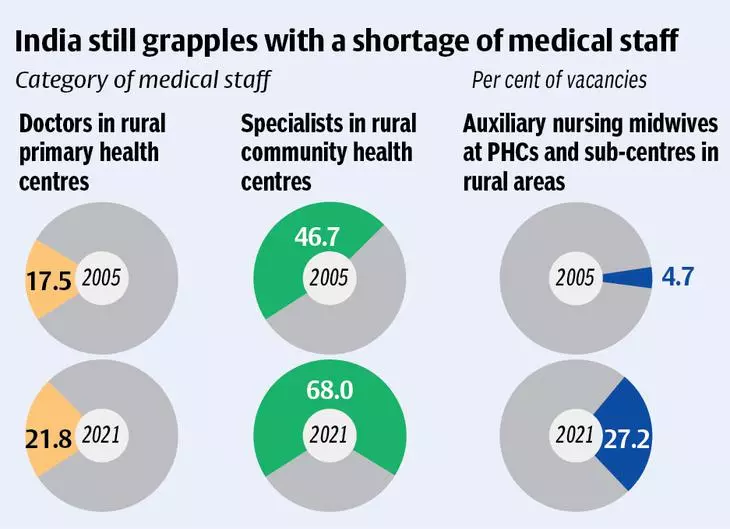
- The Rural Health Statistics report reveals an acute shortage of specialist doctors at Community Health Centers (CHCs) in India.
- Nearly 80% of the required specialists are unavailable.
- There is a shortfall of specialist doctors, including surgeons (83.2%), obstetricians and gynaecologists (74.2%), physicians (79.1%) and paediatricians (81.6%).
- The number of specialist doctors in CHCs has seen a 25% increase from 3,550 in 2005 to 4,485 in 2022.
- However, the growth in CHCs has resulted in an increased requirement for specialist doctors, creating a disparity.
- In addition to the shortage of specialist doctors, there is also a lack of female health workers and auxiliary nursing midwives in PHCs and sub-centers, with upto 14.4% of these posts lying vacant.
What are the Challenges in Addressing the Shortage of Doctors in Rural Areas?
- Inadequate Infrastructure and Resources:
- Limited healthcare facilities and resources hinder the attraction and retention of doctors in rural areas.
- Limited Access to Specialized Care:
- The scarcity of specialists in rural communities results in delayed or inadequate treatment for complex medical conditions.
- Aversion to Rural Practice:
- Doctors often prefer urban settings due to better career prospects, lifestyle preferences, and limited professional development opportunities in rural areas.
- Unequal Distribution of Medical Colleges:
- Concentration of medical colleges in urban regions leads to a lack of healthcare professionals in rural areas.
- Retention of Rural Doctors:
- Challenges in providing sufficient support, amenities, and growth opportunities make it difficult to retain doctors in rural communities.
- Socioeconomic Factors:
- Poverty, limited educational opportunities, and underdeveloped infrastructure contribute to the overall shortage of doctors in rural areas.
- Educational Disparities:
- Unequal access to quality medical education widens the gap between urban and rural healthcare services.
What are the Recent Government Initiatives Related to Healthcare?
- Accredited Social Health Activists (ASHA)
- National Health Mission
- Ayushman Bharat
- Pradhan Mantri Jan Arogya Yojana (AB-PMJAY)
- National Medical Commission
- PM National Dialysis Programme
- Janani Shishu Suraksha Karyakram (JSSK)
- Rashtriya Bal Swasthya Karyakram (RBSK)
Way Forward
- Telemedicine and Telehealth Services:
- Utilizing technology for remote consultations and medical services, bridging the gap between rural patients and healthcare providers.
- Mid-Level Healthcare Providers:
- Training and deploying physician assistants and nurse practitioners to deliver primary care services in rural areas, under the supervision of doctors.
- Rural Health Clinics and Outreach Programs:
- Establishing local healthcare facilities and mobile clinics to bring medical services directly to rural communities, improving access and convenience.
- Rural Medical Education and Residency Programs:
- Developing specialized programs to encourage medical students and residents to practice in rural areas, providing relevant training and support.
- Financial Incentives:
- Offering financial incentives and loan repayment programs to attract doctors to rural practice and alleviate financial burdens.
- Research and Data-Driven Approach:
- Continued research and data collection on rural healthcare challenges can provide valuable insights for policymaking and the implementation of targeted interventions.
- Community Engagement and Health Awareness:
- Conducting awareness campaigns to educate and empower rural communities about preventive care and the importance of healthcare utilization.
UPSC Civil Services Examination, Previous Year Questions (PYQs)
Prelims
Q. With reference to the National Rural Health Mission, which of the following are the jobs of ‘ASHA’, a trained community health worker? (2012)
- Accompanying women to the health facility for antenatal care checkup
- Using pregnancy test kits for early detection of pregnancy
- Providing information on nutrition and immunisation.
- Conducting the delivery of baby
Select the correct answer using the codes given below:
(a) 1, 2 and 3 only
(b) 2 and 4 only
(c) 1 and 3 only
(d) 1, 2, 3 and 4
Ans: (a)
Mains
Q. “Besides being a moral imperative of a Welfare State, primary health structure is a necessary precondition for sustainable development.” Analyse. (2021)