Social Justice
Noma as a Neglected Tropical Disease
- 21 Dec 2023
- 5 min read
For Prelims: Neglected Tropical disease, Cancrum oris, Gangrenous stomatitis, Noma
For Mains: Neglected Tropical Diseases, Impacts of NTDs, Initiatives for NTDs.
Why in News?
Recently, World Health Organization (WHO) added noma to its list of neglected tropical diseases (NTDs) underscoring the urgent need to address this health challenge and allocate resources for prevention and treatment.
- Noma, also known as cancrum oris or gangrenous stomatitis, is a severe gangrenous disease affecting children aged 3-10 in poor communities.
- Gangrene is a dangerous and potentially fatal condition that happens when the blood flow to a large area of tissue is cut off.
What is Noma?
- About:
- Noma, derived from the Greek "nomē" meaning "to devour," manifests as severe gangrene of the mouth and face.
- Evidence indicates that noma is caused by bacteria found in the mouth.
- This non contagious disease, exploits weakened defense with a mortality rate of around 90% and poses a significant threat to marginalized children in extreme poverty and malnutrition.
- Risk factors include poor oral hygiene, malnutrition, weakened immune systems, poverty.
- Geographic Distribution and Historical Context:
- Noma is prevalent in developing countries, especially sub-Saharan Africa, affecting poor children aged 3-10.
- Historical records show noma was reported in concentration camps during World War II and disappeared in the Western world with economic progress, emphasizing its link to poverty.
- Consequences and Treatment Challenges:
- Survivors face severe consequences like facial disfigurement, jaw muscle spasms, oral incontinence, and speech problems.
- Early detection is crucial, with therapy most effective in the disease's initial stages.
What are Neglected Tropical Diseases (NTDs)?
- NTDs are communicable diseases in tropical regions, thriving in conditions of poverty and poor healthcare access.
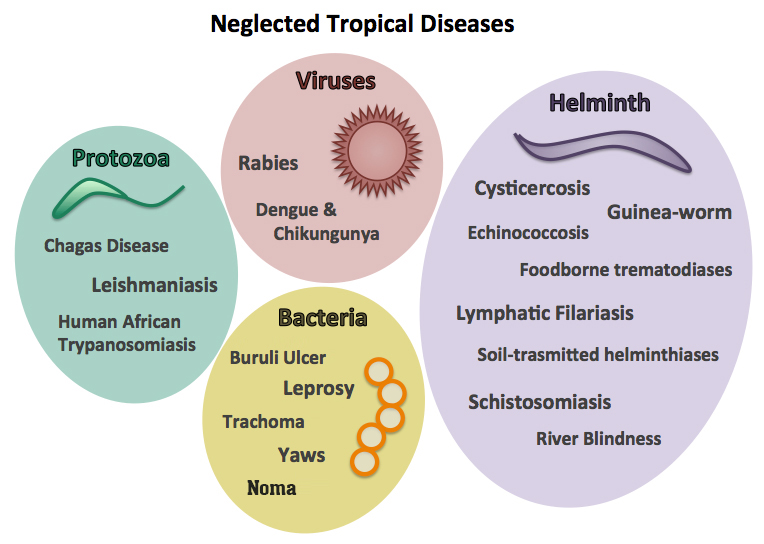
- They are caused by a variety of pathogens such as viruses, bacteria, protozoa and parasitic worms.
- The term "neglected" reflects the lack of attention and resources despite significant impact on vulnerable communities.
- These diseases generally receive less funding for research and treatment than malaises like tuberculosis, HIV-AIDS and malaria.
- Examples of NTDs are: snakebite envenomation, scabies, yaws, trachoma, Leishmaniasis and Chagas disease etc.
What is the Impact of NTDs?
- Global Scenario:
- NTDs affect more than a billion people globally. They are preventable and treatable.
- There are 20 NTDs that impact over 1.7 billion people worldwide.
- Indian Scenario:
- India carries the largest burden of at least 11 of these diseases, with parasitic illnesses like kala-azar and lymphatic filariasis affecting millions of people throughout the country – often the poorest and most vulnerable.
- India is at the cusp of eliminating Kala-Azar, with 99% Kala-Azar endemic blocks having achieved the elimination target.
What are the Initiatives for NTDs?
- Global Initiatives:
- WHO’s New Roadmap for 2021–2030:
- It is WHO’s blueprint to drive global efforts in the fight against NTDs in the context of the United Nations Sustainable Development Goals.
- The Blueprint recommends measuring impact and to promote disease-specific planning and programming
- London Declaration on NTDs: It was adopted on 30th January, 2012 to recognise the global burden of NTDs.
- WHO’s New Roadmap for 2021–2030:
- Indian Initiatives:
- The Accelerated Plan for Elimination of Lymphatic Filariasis (APELF) was launched in 2018, as part of intensifying efforts towards the elimination of NTDs.
- A WHO-supported regional alliance established by the governments of India, Bangladesh, and Nepal in 2005 to expedite early diagnosis and treatment of the most vulnerable populations and improve disease surveillance and control of sandfly populations (Kala-azar).
- India has already eliminated several other NTDs, including guinea worm, trachoma, and yaws.
- Preventive methods like Mass Drug Administration (MDA) rounds are periodically deployed in endemic areas during which anti-filarial medicines are provided free-of-cost to at-risk communities.
- Vector-control measures like Indoor Residual Spraying rounds are undertaken in endemic areas to prevent sandfly breeding.
- State and central governments have also introduced wage compensation schemes for those suffering from Kala-Azar and its sequela (a condition which is the consequence of a previous disease or injury) known as Post-Kala Azar Dermal Leishmaniasis.