Science & Technology
Tackling the Threat of Antimicrobial Resistance
- 07 Nov 2023
- 13 min read
This editorial is based on “Don’t ignore the threat of antimicrobial resistance” which was published in The Indian Express on 06/11/2023. It highlights the need for urgent action to address AMR, especially in low- and middle-income countries, where the burden of infectious diseases is high and access to quality antimicrobials is limited.
For Prelims : One Health approach, Antimicrobial Resistance (AMR’ Antibiotic Stewardship Program (AMSP), Medicines Patent Pool, Kayakalp
For Mains: Antimicrobial Resistance (AMR): Concerns, Government steps and Way Forward
The Delhi Declaration during India’s G20 presidency saw a commitment to strengthen the global health architecture by building more resilient, equitable, sustainable and inclusive health systems to implement the One Health approach, enhance pandemic preparedness and strengthen existing infectious diseases surveillance systems.
Another important part of this agreement was to prioritize tackling Antimicrobial Resistance (AMR) through research and development (R&D), infection prevention and control, as well as antimicrobial stewardship efforts within respective National Action Plans (NAPs).
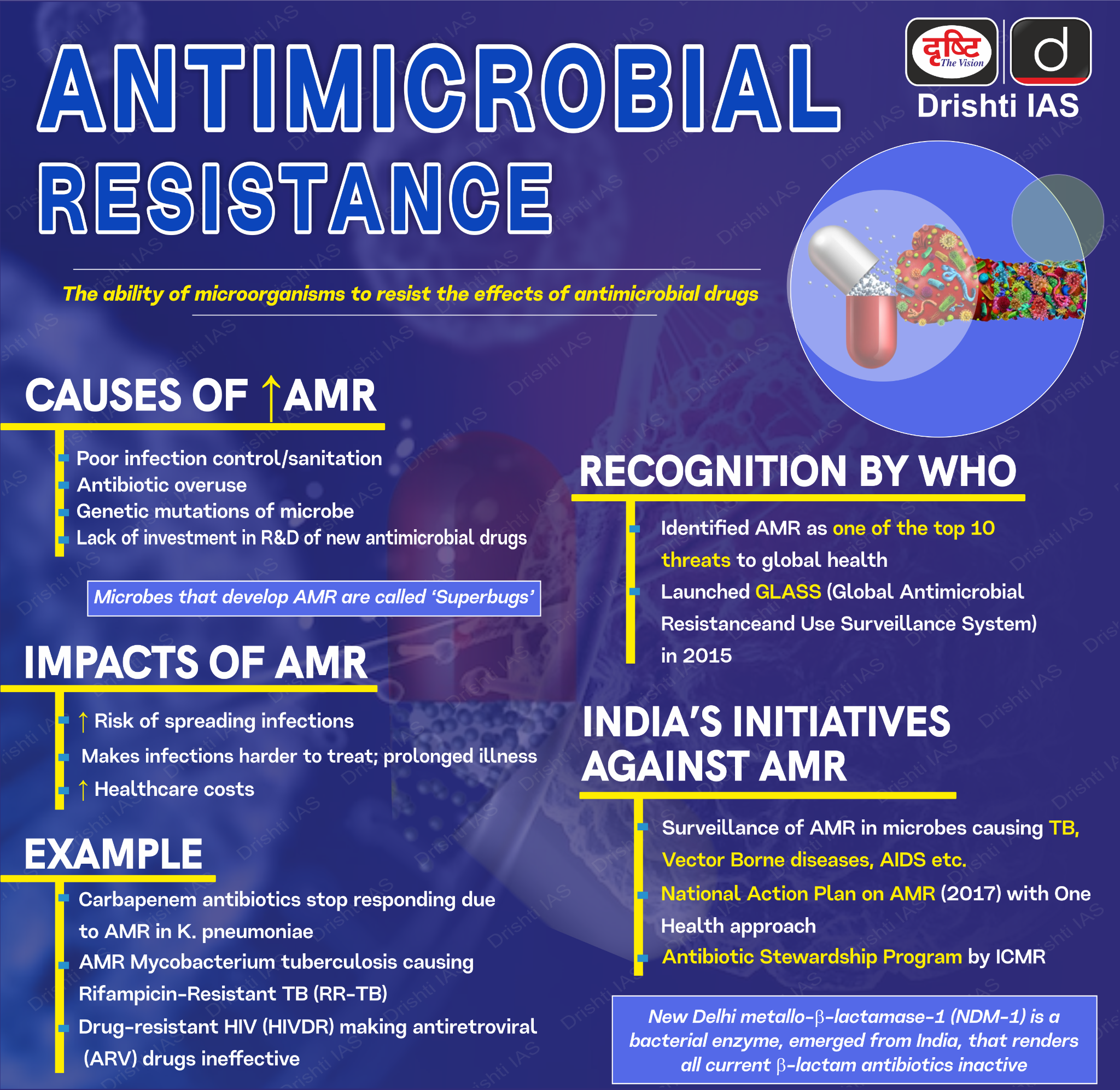
What is Antimicrobial Resistance (AMR)?
- Definition: Antimicrobial Resistance (AMR) occurs when bacteria, viruses, fungi, and parasites change over time and no longer respond to medicines, making infections harder to treat and increasing the risk of disease spread, severe illness, and death.
- Causes of AMR: Resistance in bacteria can arise naturally by genetic mutation or by one species acquiring resistance from another. It can also appear spontaneously because of random mutations or through the spreading of resistant genes through horizontal gene transfer.
- The main causes of AMR are:
- Misuse and overuse of antimicrobials
- Lack of clean water and sanitation
- Inadequate infection prevention and control
- Lack of awareness
- The main causes of AMR are:
- Health Concerns: A 2021 report by Lancet, documenting data from 204 countries, estimated that 4.95 million deaths were associated with bacterial AMR, and 1.27 million deaths were directly attributed to bacterial AMR.
- The magnitude is equal to that of diseases such as HIV and malaria.
- Sub-Saharan Africa and South Asia had the highest death rates, signifying high susceptibility to AMR.
- The rising levels of antimicrobial resistance, driven by excessive antimicrobial use threaten to compromise not only public-health gains in the field of infectious diseases but also jeopardizes cancer treatment, transplants etc.
- The magnitude is equal to that of diseases such as HIV and malaria.
- Main drivers of AMR: The main drivers of antimicrobial resistance include the misuse and overuse of antimicrobials, lack of access to clean water, sanitation, and hygiene (WASH) for both humans and animals.
What are the Concerns related to Antimicrobial resistance in India?
- High Rates of AMR: India's high rates of AMR are a serious problem. Antibiotic-resistant infections are a growing threat to public health globally. High rates of AMR can result in antibiotics becoming ineffective in treating common infections, leading to increased morbidity and mortality.
- India has one of the highest rates of AMR in the world, with more than 60,000 newborns dying each year from antibiotic-resistant infections.
- The ICMR report showed a sustained rise in drug-resistant pathogens, resulting in difficulty to treat certain infections with available medicines.
- High Burden of Infectious Diseases: India faces a significant burden of infectious diseases like tuberculosis, malaria, typhoid, cholera, and pneumonia. The emergence of AMR makes these diseases more difficult to treat effectively. It's especially concerning because these diseases are already major public health challenges in the country.
- Unregulated Antibiotic Market: The existence of a large and unregulated market for antibiotics is a major contributing factor to AMR. Overuse, misuse, and self-prescription of antibiotics can lead to the development of resistance. This issue calls for better regulation and enforcement to control the distribution and use of antibiotics.
- Lack of Surveillance and Monitoring: The absence of adequate surveillance, monitoring, and reporting systems for AMR is a significant concern. Effective monitoring and reporting are essential for tracking the spread of resistant strains and implementing appropriate interventions.
- Inadequate Infection Control Measures: The absence of infection prevention and control measures in healthcare settings is problematic. Proper infection control practices are essential to prevent the transmission of resistant infections in healthcare facilities, which can contribute to the spread of AMR.
- Limited Research and Innovation: Research and innovation in the development of new antibiotics, diagnostics, and vaccines to combat AMR are crucial. The scarcity of such efforts in India is concerning, as it limits the arsenal of tools available to combat resistant infections.
What are the Steps taken by the Government to address AMR?
- National Action Plan (NAP) for AMR: In April 2017, India's NAP for AMR was released by the Union Ministry of Health and Family Welfare. The objectives of the NAP include increasing awareness, strengthening surveillance, promoting research, and improving infection prevention and control.
- Signing the Delhi Declaration on AMR: The Delhi Declaration on Antimicrobial Resistance (AMR) is an inter-ministerial consensus that was signed by the ministers of the concerned ministries in India.
- The declaration aims to address AMR in a mission mode by involving research institutes, civil society, industry, small- and medium-sized enterprises, and encouraging public-private partnerships.
- Antibiotic Stewardship Program (AMSP): The Indian Council of Medical Research (ICMR) has initiated the AMSP on a pilot project basis in 20 tertiary care hospitals across India. The program aims to control the misuse and overuse of antibiotics in hospital wards and ICUs.
- Ban on inappropriate fixed dose combinations (FDCs): On the recommendations of the ICMR, the Drug Controller General of India (DCGI) has banned 40 FDCs that were found to be inappropriate.
- Ban on the use of Colistin as a growth promoter in animal feed: The ICMR, in collaboration with the Indian Council of Agriculture Research, Department of Animal Husbandry, Dairy and Fisheries, and the DCGI, has banned the use of Colistin as a growth promoter in animal feed in poultry.
- One Health approach: The government is working on a One Health approach by encouraging interdisciplinary collaboration at the human-animal-environmental interface. The key priority areas include zoonotic diseases, food safety, and antibiotic resistance.
- Integrated One Health Surveillance Network for AMR: The ICMR has undertaken a project on an "Integrated One Health Surveillance Network for Antimicrobial Resistance" in collaboration with the Indian Council of Agriculture Research to assess the preparedness of Indian Veterinary laboratories to participate in an integrated AMR surveillance network.
What Measures can be taken to Address the AMR issue?
- Global Efforts:
- Collaborative Action Plans: Countries, particularly G20 nations, should work together to develop regional action plans to combat AMR. These plans should include strategies for surveillance, research, and control of AMR.
- International Funding Mechanism: Establish an international funding mechanism dedicated to AMR research and development. This funding can support the creation of new antibiotics, treatment options, and technologies to combat AMR.
- Patent Reforms: Promote patent reforms to encourage innovation and affordability in new antibiotics. Models like the Medicines Patent Pool can be explored to facilitate access to necessary medications.
- Local Efforts:
- National Action Plans (NAPs) Implementation: Prioritize the implementation of National Action Plans (NAPs) related to AMR at the country level. These NAPs should include specific strategies for addressing AMR within each nation.
- Surveillance and Research: Focus on surveillance and research efforts to better understand the extent of AMR and develop innovative, affordable interventions. Expanding the scope of monitoring networks is essential to gather data and track the spread of AMR.
- Utilize Government Initiatives: Utilize government initiatives, such as Free Diagnostic Services and Kayakalp (or similar programs in other countries), to strengthen AMR containment efforts by improving healthcare services and maintaining strict protocols.
- Public Awareness and Responsible Behavior: Educate citizens about the dangers of overusing antibiotics. Encourage responsible behavior regarding antibiotic use to reduce unnecessary prescriptions and misuse.
- Involvement of Academia and Civil Society Organizations (CSOs): Engage academia to enhance understanding of the environmental dimensions of AMR, develop new technologies, and provide training and education to healthcare professionals.
- CSOs can raise awareness about AMR and advocate for policy changes, increasing public engagement in the fight against AMR.
- Benchmarking with International Examples: Benchmark with countries like Indonesia, Australia, Brazil, the UK, and the US that have implemented successful strategies to address AMR. Learn from their experiences and adapt effective measures to the local context.
- The US: The National Action Plan for Combating Antibiotic-Resistant Bacteria 2020-2025 outlines five strategic goals:
- Slowing the emergence of resistant bacteria and preventing the spread of resistant infections
- Strengthening national surveillance efforts
- Advancing the development and use of rapid and innovative diagnostic tests
- Accelerating basic and applied research and development
- Improving international collaboration and capacities.
- The UK: The UK Five Year National Action Plan for Antimicrobial Resistance 2019-2024 sets out three main ambitions: reducing the need for and unintentional exposure to antimicrobials, optimizing the use of antimicrobials, and investing in innovation, supply and access. The plan also outlines specific targets and indicators to measure progress and impact.
- The US: The National Action Plan for Combating Antibiotic-Resistant Bacteria 2020-2025 outlines five strategic goals:
|
Drishti Mains Question: Antimicrobial Resistance (AMR) threatens public health in India. Examine AMR concerns, government efforts, and suggest more actions to combat it. |
UPSC Civil Services Examination Previous Year’s Question (PYQs)
Q. Which of the following are the reasons for the occurrence of multi-drug resistance in microbial pathogens in India? (2019)
- Genetic predisposition of some people
- Taking incorrect doses of antibiotics to cure diseases
- Using antibiotics in livestock farming
- Multiple chronic diseases in some people
Select the correct answer using the code given below.
(a) 1 and 2
(b) 2 and 3 only
(c) 1, 3 and 4
(d) 2, 3 and 4
Ans: (b)
Q. Can overuse and free availability of antibiotics without Doctor’s prescription be contributors to the emergence of drug-resistant diseases in India? What are the available mechanisms for monitoring and control? Critically discuss the various issues involved. (2014)