Social Issues
WHO Guidelines on Antimicrobial Resistance (AMR)
- 11 Sep 2024
- 9 min read
For Prelims: World Health Organization (WHO), Antibiotic Resistance, Pharmaceutical Manufacturing, Generic Drugs, Active Pharmaceutical Ingredients (APIs), Bacteria, Viruses, Fungi, Parasites, World Bank, Broad-Spectrum Antibiotics, Pneumonia.
For Mains: Rising threat of antimicrobial resistance (AMR) and their impact.
Why in News?
Recently, the World Health Organization (WHO) published “Guidance on wastewater and solid waste management for manufacturing of antibiotics” to tackle the threat of Antimicrobial Resistance (AMR).
What are the Key Highlights of the Guidance?
- About: The document provides a scientific framework for regulators, industry, and other stakeholders to effectively control antibiotic resistance.
- Objective: The guidance aims to offer a scientific foundation for setting and incorporating targets into policies and regulations to prevent antibiotic resistance.
- Non-binding Nature: The guidance is not legally binding. However, it helps ensure consistency across policies and market instruments, promoting transparency and avoiding fragmented approaches.
- Principles and Best Practices:
- Risk Management Plans: Includes best practices for developing risk management plans, based on proven methods in other sectors like food and water safety.
- Audit and Transparency: Emphasises the importance of internal and external audits and public transparency.
- Progressive Implementation: Encourages a stepwise approach with progressive improvement, recognising the need for global supply protection and equitable access to quality antibiotics.
- Target Audiences:
- Regulatory Bodies: National or regional authorities responsible for overseeing pharmaceutical manufacturing and waste management.
- Third-party organisations conducting audits and inspections of antibiotic production and waste management.
- Generic Substitution and Reimbursement Entities: Bodies responsible for decisions related to generic drugs and their reimbursement.
- Industrial Actors: Companies involved in any stage of antibiotic production and their collective organisations.
- Waste Management Services: Entities managing the disposal of antibiotic waste and wastewater.
- Regulatory Bodies: National or regional authorities responsible for overseeing pharmaceutical manufacturing and waste management.
- Scope of the Guidance:
- Human Health-Based Targets: Focuses on reducing the risk of antibiotic resistance.
- Ecotoxicological Risks: Addresses risks to aquatic life from antibiotic pollution.
- Coverage: Includes all stages of antibiotic production, from manufacturing active pharmaceutical ingredients (APIs) to finished products and primary packaging.
- Waste Focus: Applies to both liquid and solid waste, emphasising liquid effluents, run-offs, and land discharges.
- Assessment Needs: Requires separate risk assessments for manufacturing sites producing multiple APIs or products, considering both pre- and post-dilution risks in water bodies and the release of resistant bacteria.
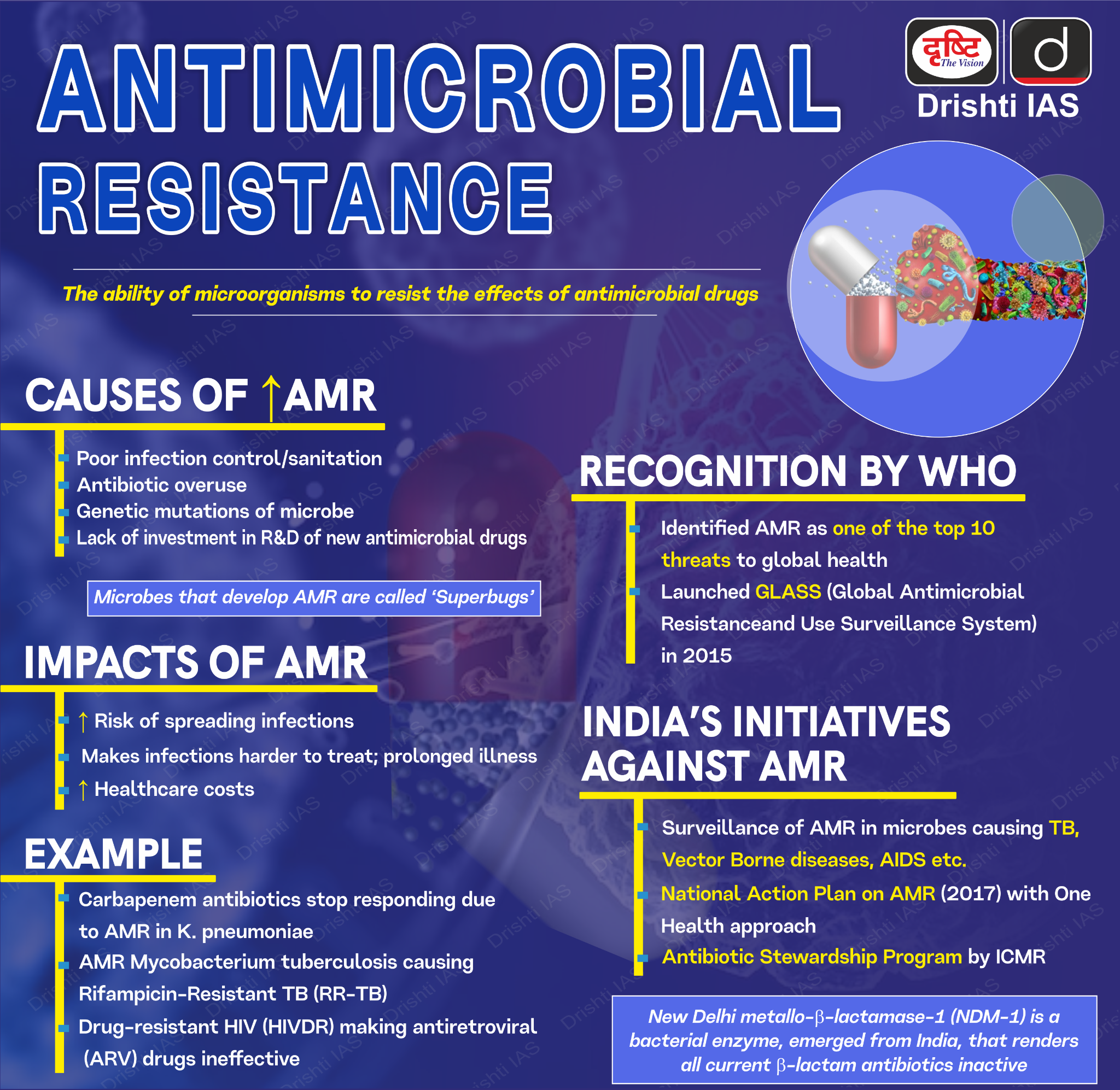
What is Antimicrobial Resistance (AMR)?
- About AMR: AMR occurs when bacteria, viruses, fungi and parasites no longer respond to antimicrobial medicines.
- As a result of drug resistance, antibiotics and other antimicrobial medicines become ineffective and infections become difficult or impossible to treat, increasing the risk of disease spread, severe illness, disability and death.
- Prevalence of AMR: AMR is one of the top global public health and development threats.
- It is estimated that bacterial AMR was directly responsible for 1.27 million global deaths in 2019 and contributed to 4.95 million deaths.
- Economic Cost of AMR: The World Bank estimates that AMR could result in USD 1 trillion additional healthcare costs by 2050.
- It can lead to USD 1 trillion to USD 3.4 trillion gross domestic product (GDP) losses per year by 2030.
- Reasons for Increasing AMR:
- Individual Practices: Many people have a tendency to use antibiotics even for viral infections. An antibiotic is of no use for viral infections such as influenza, but consuming it can drive up resistance in the population.
- Medical Practices: Doctors prescribe broad-spectrum antibiotics that work against a wide range of infections.
- Overuse of broad-spectrum antibiotics leads to increased resistance as antibiotics may not be required in the body.
- Diagnostic Challenges: Doctors often prescribe antibiotics based on symptoms alone instead of prescribing diagnostic tests to identify the exact cause of the infection.
- Pharmaceutical Manufacturing: Pharmaceutical waste from antibiotic manufacturing can facilitate the emergence of new drug-resistant bacteria, which can spread globally and threaten our health.
- Common Resistant Pathogens in India:
- E. Coli (Gut infections): It demonstrated a decrease in susceptibility to most antibiotics, with susceptibility to carbapenem (antibiotics) reducing from 81.4% in 2017 to 62.7% in 2023.
- Klebsiella Pneumoniae (Pneumonia and Urinary Tract Infections): Its susceptibility to two different medicines from the carbapenem class reduced from 58.5% to 35.6% and 48% to 37.6% between 2017 and 2023.
- Acinetobacter Baumannii (Hospital Acquired Infections): While no significant change was found in susceptibility, it is highly resistant to even strong antibiotics.
How can AMR be Tackled?
- Public Awareness Campaign: A well-executed long-term public campaign could significantly reduce antimicrobial prescriptions by addressing patient demands and over-the-counter purchases.
- Improved Sanitation: Enhanced sanitation measures, like regular handwashing, waste management, and clean surroundings, help break the chain of transmission of both common and resistant pathogens.
- Reduce Unnecessary Use of Antimicrobials: Doctors should ensure appropriate use of antibiotics and reserve the more potent ones for hospital based patients.
- Promote New and Rapid Diagnostics: Develop and use rapid diagnostic tests to avoid unnecessary antibiotic prescriptions.
- Vaccine Development and Alternative Therapies: Investing in new vaccines and alternatives like phage therapy, probiotics, and antibodies will help reduce antibiotic dependency.
- New Drug Development: Incentivizing pharmaceutical companies to develop new antibiotics is essential, given the uncertainties and current effectiveness of existing treatments.
|
Drishti Mains Question: Q. Critically examine the primary causes of Antimicrobial resistance and discuss the multifaceted strategies needed to combat its rise. |
UPSC Civil Services Examination, Previous Year Questions (PYQ)
Prelims
Q. What is the importance of using Pneumococcal Conjugate Vaccines in India? (2020)
- These vaccines are effective against pneumonia as well as meningitis and sepsis.
- Dependence on antibiotics that are not effective against drug-resistant bacteria can be reduced.
- These vaccines have no side effects and cause no allergic reactions.
Select the correct answer using the code given below:
(a) 1 only
(b) 1 and 2 only
(c) 3 only
(d) 1, 2 and 3
Ans: (b)
Q. Which of the following are the reasons for the occurrence of multi-drug resistance in microbial
- pathogens in India? (2019)
- Genetic predisposition of some people
- Taking incorrect doses of antibiotics to cure diseases
- Using antibiotics in livestock farming
- Multiple chronic diseases in some people
Select the correct answer using the code given below.
(a) 1 and 2
(b) 2 and 3 only
(c) 1, 3 and 4
(d) 2, 3 and 4
Ans: (b)
Q. Widespread resistance of malarial parasite to drugs like chloroquine has prompted attempts to develop a malarial vaccine to combat malaria. Why is it difficult to develop an effective malaria vaccine?(2010)
(a) Malaria is caused by several species of Plasmodium
(b) Man does not develop immunity to malaria during natural infection
(c) Vaccines can be developed only against bacteria
(d) Man is only an intermediate host and not the definitive host
Ans: (b)
Mains
Q. Can overuse and free availability of antibiotics without Doctor’s prescription, be contributors to the emergence of drug-resistant diseases in India? What are the available mechanisms for monitoring and control?Critically discuss the various issues involved. (2014)