Science & Technology
India’s AMR Crisis
- 28 May 2025
- 12 min read
For Prelims: Antimicrobial Resistance (AMR), Nafithromycin, Superbugs, WHO, Broad-spectrum Antibiotics, National Action Plan on AMR, National Centre for Disease Control (NCDC), Red Line Campaign, Fixed-dose Combination (FDC), Schedule H1 Drugs, GLASS (Global Antimicrobial Resistance Surveillance System).
For Mains: Antimicrobial Resistance, their implications, Steps taken and additional measures needed to curb AMR.
Why in News?
The launch of Nafithromycin (Miqnaf)—India’s first indigenously developed antibiotic in over 30 years, marks a key step in combating Antimicrobial Resistance (AMR), but the scale and urgency of the AMR crisis demand far broader and sustained efforts.
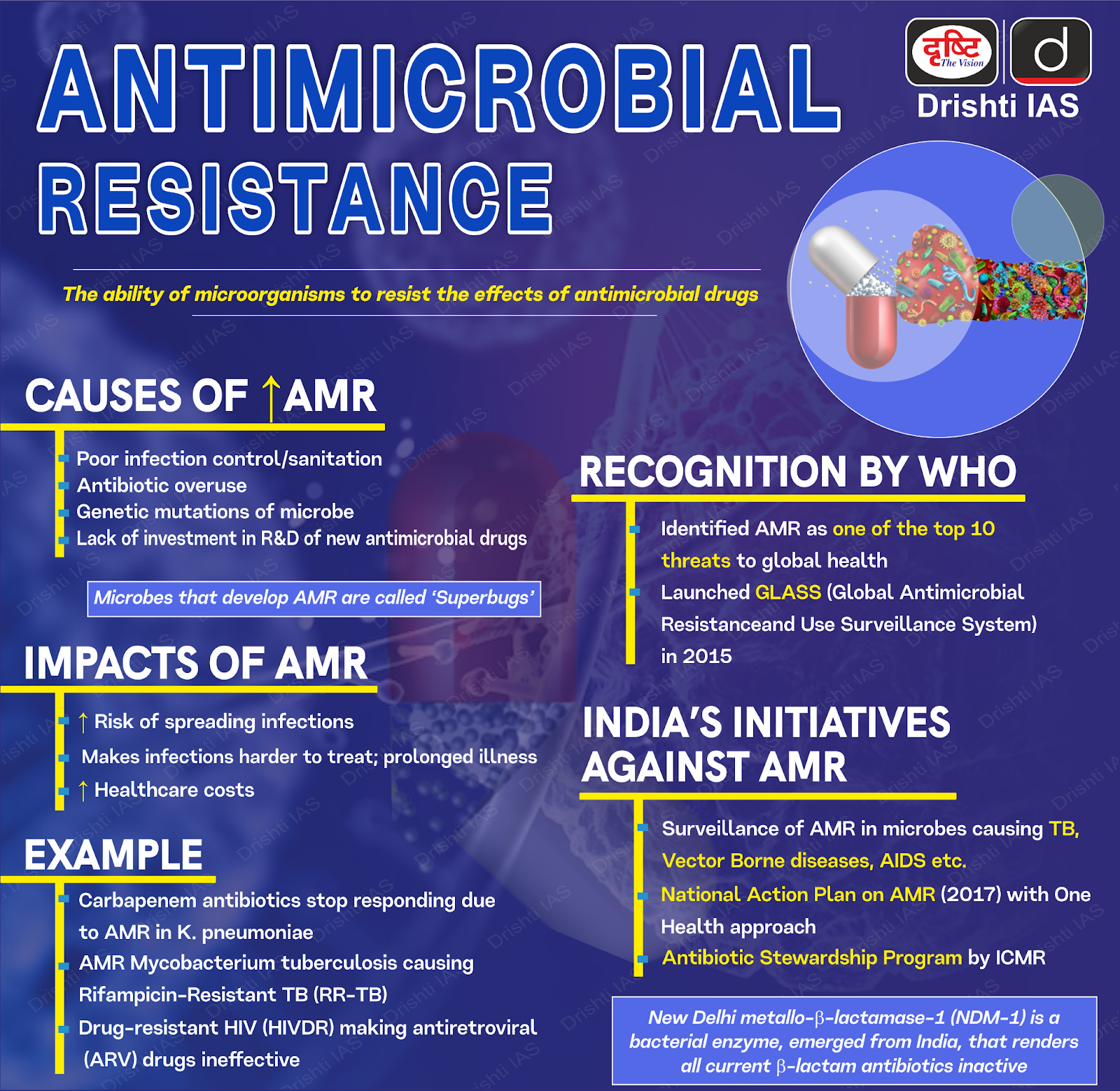
What is Antimicrobial Resistance (AMR)?
- About: AMR occurs when microorganisms (bacteria, viruses, fungi, parasites) adapt and resist drugs like antibiotics and antivirals, making infections harder to treat and easier to spread.
- Threat: A 2019 report by the Institute of Health Metrics and Evaluation (IHME) revealed that AMR caused 2,97,000 deaths in India and 1.27 million globally.
- If unchecked, The Lancet projects 1.91 million direct AMR deaths and 8.22 million associated deaths by 2050.
What are the Key Issues Leading to Rise of AMR in India?
- Overuse of Antibiotics: Improper prescriptions and overuse of antibiotics—even for viral infections like influenza—drives resistance.
- Although only 30% of antibiotics are used in humans, in 2022, 59% of India’s antibiotic consumption came from the "Watch" group.
- The "Watch" group is a category of antibiotics classified by the World Health Organization (WHO), intended for use only in treating severe infections.
- Although only 30% of antibiotics are used in humans, in 2022, 59% of India’s antibiotic consumption came from the "Watch" group.
- Inadequate Healthcare Infrastructure: Lack of diagnostic tools leads doctors to prescribe broad-spectrum antibiotics empirically. Overcrowded, unhygienic hospitals and poor infection control promote resistant bacteria and hospital-acquired infections.
- Frequent AMR outbreaks in Indian tertiary care centers highlight systemic deficiencies fueling antimicrobial resistance (AMR) .
- Lack of New Antibiotics: No new antibiotics emerged for 30 years until Nafithromycin (2024), as pharma companies prioritize more profitable chronic disease drugs over antibiotic R&D.
- Unregulated Use in Agriculture and Animal Husbandry: India is among the top antibiotic consumers in livestock, where 70% are used for growth promotion in livestock, agriculture, and aquaculture.
- These antibiotics enter the food chain and environment, spreading resistance. Indiscriminate antibiotic use in aquaculture further worsens the problem.
- Environmental Factors: Pharmaceutical factories discharge antibiotic residues into water bodies without proper treatment, contaminating rivers and soil, and creating resistance hotspots.
- Inadequate sewage and waste management in India further allow resistant microbes to spread unchecked in the environment.
What are the Consequences of Rising Antimicrobial Resistance?
- Health Catastrophe: AMR makes infections harder to treat, raising mortality and morbidity. Common illnesses like tuberculosis, pneumonia, and urinary tract infections can become life-threatening.
- E.g., In 2017, multidrug-resistant or rifampicin-resistant TB caused 230,000 deaths, mostly in India and China.
- Surgeries, chemotherapy, and transplants depend on effective antibiotics; without them, routine procedures become high-risk.
- Economic Cost: The World Bank estimates AMR could add USD 1 trillion in healthcare costs by 2050 and cause USD 1–3.4 trillion in annual GDP losses by 2030.
- Longer illnesses and deaths lower workforce efficiency, while livestock losses disrupt food chains.
- Food Security Crisis: With 70% of antibiotics used in farming, the AMR accelerates threatening food availability, quality, and safety, and posing a risk to national food security.
- E.g., Resistant E. coli in poultry can infect humans, and antifungal-resistant blights harm crops like wheat, rice, and bananas.
- Environmental Spread: Drug waste, hospital sewage, and farm runoff spread resistance genes, while migratory birds and marine life carry resistant bacteria worldwide.
- E.g., the River Ganga carries superbug bacterial genes, exposing users to antibiotic-resistant infections.
- Social Implications: Poorer communities and countries with limited healthcare face higher AMR deaths due to scarce diagnostics and drugs, risking declining public confidence in treatments.
What Measures are Underway to Tackle Antimicrobial Resistance in India?
- National Action Plan on AMR (2017): NAP on AMR aligns with global efforts, focusing on surveillance, rational antibiotic use, and public awareness.
- Coordinated by the National Centre for Disease Control (NCDC), it covers 50 medical colleges/labs across 27 states and 6 UTs as of March 2024.
- AMR Surveillance Networks: Through the National Antimicrobial Surveillance Network (NARS-Net), India monitors nine priority bacterial pathogens, including Escherichia coli.
- Antibiotic Regulation: In August 2024, the government banned 156 fixed-dose combination (FDC) drugs, including popular medicines such as Cheston Cold and Foracet.
- Hospital Antimicrobial Stewardship Programs (AMSP) optimize patient care and help combat antimicrobial resistance.
- Schedule H1 drugs (last-resort antibiotics e.g., carbapenems) require chemists to retain prescription copies before sale.
- In January 2024, Kerala became the first state in India to ban the over-the-counter sale of antibiotics without a prescription, setting an example that other states can follow to reduce antibiotic misuse.
- Research & Innovation: Centre for Cellular and Molecular Platforms (C-CAMP) India AMR Challenge identifies and supports startups, companies, and innovators developing technologies to tackle AMR.
- Companies like Wockhardt, Orchid Pharma, and Bugworks are among the few in India focusing on antibiotic development.
- Public Awareness: Red Line Campaign warns against using medicines marked with a vertical red line, including antibiotics, without a prescription.
- Global Collaboration: India participates in WHO's GLASS (Global Antimicrobial Resistance Surveillance System) to standardize and strengthen the collection, analysis, and sharing of data on AMR across countries.
What Further Measures Should be Adopted to Combat AMR?
- Strengthening Regulations: Enforce Schedule H1 to ban over-the-counter antibiotic sales with prescription retention, expand the colistin (growth promoter in the poultry industry) ban on non-therapeutic antibiotics in livestock, and regulate pharmaceutical antibiotic discharge into water bodies.
- India must strengthen the Drug and Cosmetics Act to penalize unauthorized antibiotic sales and enforce prescription audits.
- Domestic Antibiotic Development: Government must incentivize pharma through tax breaks & grants (like BIRAC’s support for Nafithromycin) and expand initiatives like C-CAMP AMR Challenge to support startups (e.g., Bugworks).
- Enhancing Antibiotic Stewardship Programs: Hospitals and clinics must implement antibiotic stewardship programs to optimize prescription and usage, supported by training on rational use and regular prescription audits.
- Incorporating stewardship into medical education and professional development ensures sustainable change.
- Use machine learning for real-time AMR tracking and isolate AMR patients to prevent outbreaks.
- Expanding and Upgrading Diagnostic Facilities: Improved access to affordable, rapid diagnostic tests helps confirm bacterial infections before prescribing antibiotics, preventing unnecessary use.
- Investing in point-of-care diagnostics at rural and primary health centers reduces guesswork and supports targeted therapy.
- Public Awareness: Expand Red Line awareness to include AMR risks in livestock and agriculture, with ASHA workers educating rural communities and farmers attending workshops on reducing antibiotic use in poultry and aquaculture.
- Promoting One Health Approach: Promote multisectoral collaboration across health, veterinary, agriculture, and environment sectors and enforce stricter regulations on antibiotic use in livestock and agriculture to reduce misuse and contamination.
Conclusion
The launch of Nafithromycin marks a significant milestone, but combating AMR requires a multifaceted, sustained approach. Strengthening regulations, fostering One Health collaboration, boosting domestic antibiotic innovation, enhancing rapid diagnostics and hospital stewardship, and expanding public awareness are crucial to curb resistance and safeguard global health security.
|
Drishti Mains Question: Q. Discuss the causes of Antimicrobial Resistance (AMR) in India and suggest a comprehensive strategy to combat it. |
UPSC Civil Services Examination, Previous Year Questions (PYQ)
Prelims
Q. What is the importance of using Pneumococcal Conjugate Vaccines in India? (2020)
- These vaccines are effective against pneumonia as well as meningitis and sepsis.
- Dependence on antibiotics that are not effective against drug-resistant bacteria can be reduced.
- These vaccines have no side effects and cause no allergic reactions.
Select the correct answer using the code given below:
(a) 1 only
(b) 1 and 2 only
(c) 3 only
(d) 1, 2 and 3
Ans: (b)
Q. Which of the following are the reasons for the occurrence of multi-drug resistance in microbial pathogens in India? (2019)
- Genetic predisposition of some people
- Taking incorrect doses of antibiotics to cure diseases
- Using antibiotics in livestock farming
- Multiple chronic diseases in some people
Select the correct answer using the code given below.
(a) 1 and 2
(b) 2 and 3 only
(c) 1, 3 and 4
(d) 2, 3 and 4
Ans: (b)
Mains
Q. Can overuse and free availability of antibiotics without Doctor’s prescription, be contributors to the emergence of drug-resistant diseases in India? What are the available mechanisms for monitoring and control? Critically discuss the various issues involved. (2014)