West Nile Virus | 01 Jun 2022
For Prelims: West Nile Virus, Flavivirus, Transmission cycle of West Nile Virus, WHO
For Mains: Prevention and Control of virus-associated diseases
Why in News?
Recently, a 47-year-old man in Thrissur, Kerala died due to West Nile Virus (WNV). This has caused the Kerala health department to be on alert.
- Malappuram’s 6-year-old boy also died of the same infection, earlier in 2019.
- WNV was first reported in the state of Alappuzha in 2006. Later in 2011, it was also reported in Ernakulam, Kerala.
What is WNV?
- About:
- The West Nile Virus is a flavivirus related to the viruses that are also responsible for causing St. Louis encephalitis, Japanese encephalitis, and yellow fever.
- It is a mosquito-borne, single-stranded RNA virus.
- Global Prevalence:
- Along all major bird migratory routes, WNV outbreak sites are found.
- Africa, Europe, the Middle East, North America, and West Asia are the regions where the virus is commonly found.
- Usually, WNV infections peak during the period when mosquito vectors are most active and the ambient temperature is high enough for virus multiplication for most of the countries.
- Prevalence in India:
- In Mumbai in the year 1952, the antibodies against WNV were first detected in humans.
- Since then, the virus activity has been reported in southern, central, and western India.
- In Andhra Pradesh and Tamil Nadu, WNV was isolated from Culex vishnui mosquitoes.
- In Maharashtra, it was isolated from Culex quinquefasciatus mosquitoes.
- In Karnataka, it has been isolated from humans.
- Further, WNV neutralizing antibodies were found to be present in human serum collected from Tamil Nadu, Karnataka, Andhra Pradesh, Maharashtra, Gujarat, Madhya Pradesh, Odisha, Rajasthan and Assam.
- In 1977, 1978 and 1981, serologically confirmed cases of WNV infections were reported in Vellore and Kolar districts, and in West Bengal in 2017.
- During an acute encephalitis outbreak in Kerala, the complete genome sequence of WNV was isolated in 2013.
- The association of WNV with eye infection in Tamil Nadu had been clearly established during an epidemic of mysterious fever in the first half of 2010.
- Origin:
- WNV was first isolated in a woman in the West Nile district of Uganda in 1937.
- It was identified in birds in the Nile delta region in 1953. Before 1997, WNV was not considered pathogenic for birds.
- Human infections attributable to WNV have been reported in many countries for over 50 years.
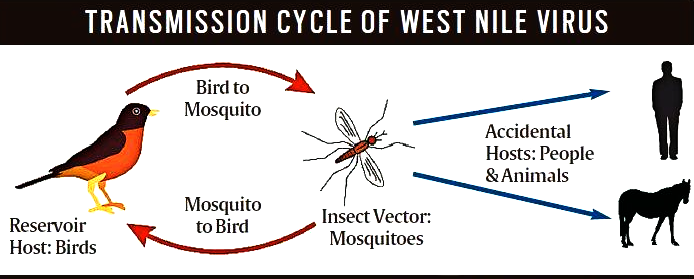
- Transmission Cycle:
- Principal vector for transmission is the culex species of mosquitoes.
- Birds act as the reservoir host of the virus.
- Infected mosquitoes transmit WNV between and among humans and animals, including birds.
- When a mosquito feeds on infected birds, they become infected.
- The virus circulates in the blood of those infected mosquitoes for a few days, eventually getting into the mosquito’s salivary glands.
- The virus may get injected into humans and animals during later blood meals (when mosquito bites). Therein, WNV can multiply and possibly cause illness.
- WNV can also get transmitted from an infected mother to her child through blood transfusion or via exposure to the virus in laboratories.
- No instance of transmission by contact with infected humans or animals has been reported.
- It does not spread “through eating infected animals, including birds.
- Generally, the incubation period for WNV disease is 2-6 days. However, this may range from 2-14 days, and can also be several weeks in people whose immunity is compromised.
- According to the World Health Organization (WHO), no human-to-human transmission of WNV through casual contact has been reported till date.
- Symptoms:
- In 80% of the infected people, the disease is asymptomatic.
- In the rest of the 20% cases, West Nile fever or severe WNV is observed with symptoms such as fever, headache, fatigue, body aches, nausea, rash, and swollen glands.
- Severe infection may even cause neurological diseases like West Nile encephalitis or meningitis or West Nile poliomyelitis or acute flaccid paralysis.
- Also, there are reports of WNV-associated Guillain-Barré syndrome and radiculopathy.
- Around 1 in 150 individuals with WNS is likely to develop a more severe form of disease.
- It may take several weeks or months to recover from severe illness.
- Nervous system damage can last forever.
- In persons with co-morbidities and immuno-compromised persons (such as transplant patients), the disease may turn out to be fatal.
- Measures of Prevention:
- The establishment of an active animal health surveillance system to detect new cases in birds and horses should be essentially established.
- As WNV outbreaks in animals precede human cases, it is necessary to provide early warning for veterinary and human public health authorities.
- The European Centre for Disease Control and Prevention (ECDC) has suggested that 28-day blood donor deferral or nucleic acid testing of prospective donors who have visited or lived in an affected area should be implemented by the European Union (EU).
- Besides, testing for WNV infection must be done for the donors of organs, tissues and cells, who are living in or returning from an affected area.
- Treatment:
- As of now, no treatment/vaccine for WNV is available.
- Only supportive treatments can be provided to neuroinvasive WNV patients.
UPSC Civil Services Examination, Previous Year Question
Q. Consider the following statements: (2017)
- In tropical regions, Zika virus disease is transmitted by the same mosquito that transmits dengue.
- Sexual transmission of Zika virus disease is possible.
Which of the statements given above is/are correct?
(a) 1 only
(b) 2 only
(c) Both 1 and 2
(d) Neither 1 nor 2
Ans: (c)
Exp:
- Zika virus is a flavivirus which was first discovered in 1947 in monkeys and then in humans in Uganda in 1952.
- Both Zika and Dengue have similarities in terms of symptoms of fever, skin rashes, conjunctivitis, muscle and joint pain, malaise, and headache. In addition to this, the mode of transmission is also same for both the diseases, i.e., both are spread by Aedes aegypti and Aedes albopictus species of mosquitoes. Hence, statement 1 is correct.
- Modes of Zika Transmission:
- Mosquito bites
- From mother to child during pregnancy, which can cause microcephaly and other severe fetal brain defects. Zika virus has also been found in breast milk.
- Sexual transmission from infected partner. Hence, statement 2 is correct.
- Through blood transfusion.
- Therefore, option (c) is the correct answer.