Passive Euthanasia in India | 08 Oct 2025
For Prelims: Euthanasia, Article 21, Bharatiya Nyaya Sanhita
For Mains: Constitutional Right to Die with Dignity under Article 21,Ethical principles in medical decision-making: Autonomy, Beneficence, Justice
Why in News?
In June 2025, the UK’s House of Commons passed the Terminally Ill Adults (End of Life) Bill, which allows passive euthanasia and has now revived the global debate on the right to die with dignity.
- India recognises passive euthanasia through Supreme Court (SC) of India rulings, but its challenging implementation underscores the need to reform the framework to uphold the constitutional promise of dignity in death.
What is Euthanasia?
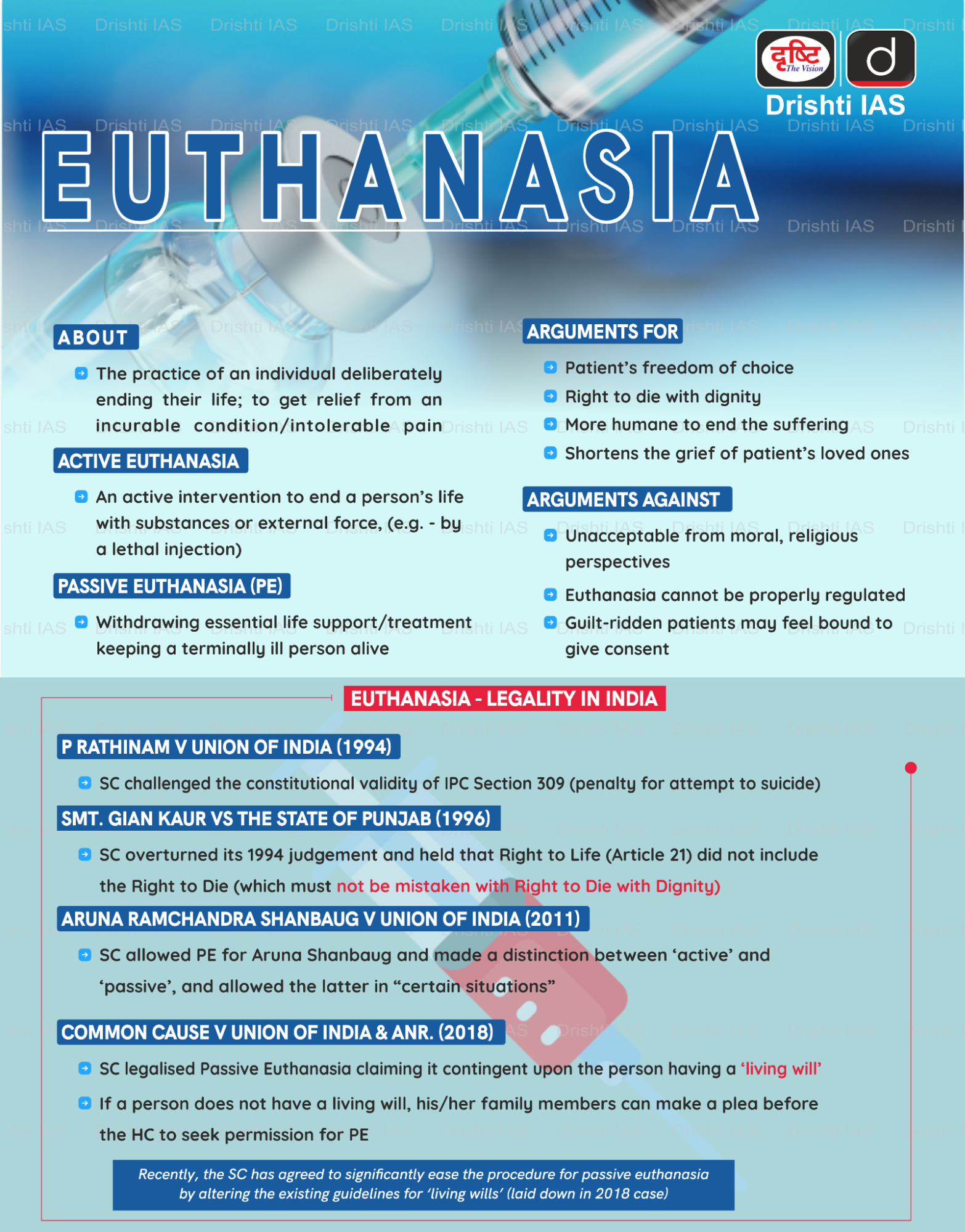
- About: Euthanasia or “mercy killing” refers to deliberately hastening a person’s death to prevent further suffering from incurable or terminal illness.
- Types of Euthanasia:
- Active euthanasia: Directly causing a patient’s death, such as through a lethal injection.
- Forms of active euthanasia include:
- Voluntary: Patient consciously chooses death.
- Non-voluntary: Decision made for an incompetent patient.
- Involuntary: Death caused without consent.
- Forms of active euthanasia include:
- Passive euthanasia: The withdrawal or withholding of life-support or medical treatment when a patient is terminally ill and has no realistic chance of recovery, allowing death to occur naturally.
- This aims to protect the right to die with dignity and prevent prolonged, futile suffering in irreversible medical conditions.
- Active euthanasia: Directly causing a patient’s death, such as through a lethal injection.
- Legal Status in India:
- Active Euthanasia: It is illegal in India. The Bharatiya Nyaya Sanhita (BNS), 2023 classifies acts committed with the intention of causing death as culpable homicide or murder under Sections 100 and 101.
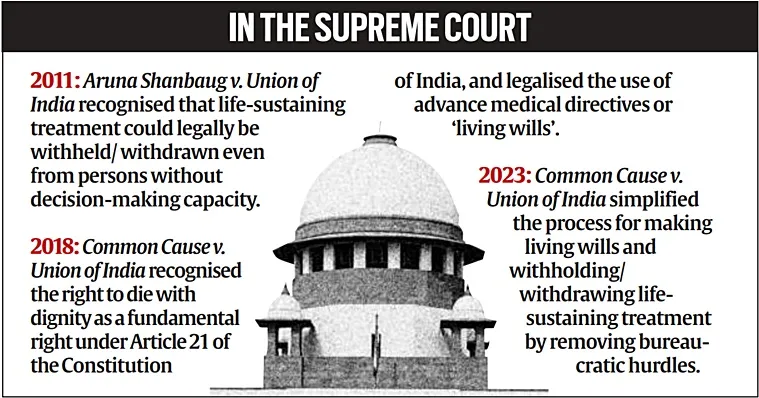
- Passive Euthanasia: In Aruna Shanbaug v. Union of India (2011), the SC recognized that life-sustaining treatment could legally be withheld or withdrawn. It applies even to persons without decision-making capacity.
- In Common Cause v. Union of India (2018), the SC recognized the right to die with dignity as a fundamental right under Article 21 of the Constitution, and legalized the use of advance medical directives or “living wills (specifying conditions under which treatment may be withdrawn)”.
- Supreme Court Guidelines on Euthanasia: The Supreme Court in 2023 modified the 2018 Euthanasia Guidelines to ease the process of granting passive euthanasia.
-
Living Wills / Advance Directives: Adults of sound mind can create a living will. It must be signed by the executor in the presence of two witnesses.
-
Signature can be attested by a notary or gazetted officer.
-
-
Medical Board Approval: Hospital forms two medical boards. Medical boards must communicate their decision within 48 hours.
-
High Court Oversight: If hospital boards deny permission, the patient’s kin can approach the High Court, which forms a fresh medical board to review the case.
-
-
Global Perspective: Passive euthanasia is accepted in many countries. Countries like the Netherlands and Belgium have legalised active euthanasia under strict safeguards.
Did you Know?
- Euthanasia and assisted suicide are not the same. Euthanasia involves another person, usually a doctor, directly ending a patient’s life. Assisted suicide involves providing the means or information for a person to end their own life.
- Suicide tourism, also called euthanasia tourism, refers to patients traveling to countries where euthanasia or assisted suicide is legal.
- Switzerland is the leading destination, attracting patients primarily from the UK, Germany, and France.
What are the Ethical Perspectives of Euthanasia?
- Autonomy (Self-Determination): Patients should have the right to make informed choices about their life and death.
-
Supports passive euthanasia, allowing terminally ill patients to refuse life-prolonging treatment.
-
-
Beneficence (Acting in Patient’s Best Interest): Medical actions should aim to relieve suffering.
-
Passive euthanasia aligns with this principle by withdrawing futile treatment.
-
-
Justice (Fairness and Equity): Ensures equitable access to palliative care and legal safeguards.
-
Vulnerable patients must not be pressured into active or passive euthanasia due to financial or social constraints.
-
Why is there a Need to Reform Passive Euthanasia in India?
- Bureaucratic Delays: The modified 2018 euthanasia guidelines aim to fast-track passive euthanasia, but due to ineffective implementation, current procedures involving multi-tier approvals still cause delays for terminally ill patients, prolonging suffering and undermining the constitutional promise of dignity in death.
- Practical Inaccessibility: Families and doctors often bypass legal procedures due to their complexity, leaving decisions informal and exposing medical professionals to potential legal liability.
- Low Awareness: Many patients, families, and healthcare professionals are unaware of legal provisions such as living wills and advance directives, limiting the practical use of passive euthanasia.
- Societal and Cultural Concerns: In India, euthanasia is often viewed with moral opposition due to the belief in the sanctity of life, as well as religious and cultural perspectives that consider it akin to murder.
- Fragmented Healthcare System: Uneven hospital infrastructure, lack of trained personnel, and absence of hospital-level ethics committees prevent timely, fair, and humane implementation of passive euthanasia.
What Reforms are Needed for Passive Euthanasia in India?
- Digitisation of Advance Directives: Create a National Euthanasia Portal linked with Aadhaar for registering, updating, or revoking living wills.
- Allow doctors to validate mental capacity online, reducing paperwork and delays.
- Hospital-Level Ethics Committees: Establish committees including senior physicians, palliative care specialists, and an independent member.
- Empower them to authorize withdrawal of life support within 48 hours, decentralizing decision-making.
- Transparent Oversight: Replace single-state ombudsman model with digital dashboards or state-level health commissioners to monitor cases.
- Conduct periodic audits and public reporting to build trust and prevent misuse.
- Mandatory Safeguards: Include 7-day cooling-off period, psychological counselling, and palliative care review before approving withdrawal of treatment.
- Protect vulnerable populations (elderly, disabled, financially dependent) from coercion.
- Capacity Building & Awareness: Integrate end-of-life ethics and legal training into medical and nursing curricula.
- Run public awareness campaigns to normalize living wills, advance care planning, and palliative care options.
- Streamlined Procedures: Simplify approvals while maintaining safeguards to reduce bureaucratic delays and ensure timely relief for terminally ill patients.
Conclusion
Reforming passive euthanasia is crucial to make the law workable, ethical, and aligned with India’s constitutional commitment to dignity in dying, bridging the gap between legal recognition and practical access.
|
Drishti Mains Question: Q. Examine the ethical and legal challenges surrounding passive euthanasia in India and suggest reforms to ensure the constitutional promise of dignity in death |
Frequently Asked Questions (FAQs)
- What is passive euthanasia?
Passive euthanasia involves withholding or withdrawing life-support or medical treatment from terminally ill patients, allowing natural death while protecting the right to die with dignity. - Is active euthanasia legal in India?
No. Active euthanasia is illegal under the Bharatiya Nyaya Sanhita (BNS) as it is considered culpable homicide or murder. - Which Supreme Court cases recognised passive euthanasia in India?
Aruna Shanbaug v. Union of India (2011) and Common Cause v. Union of India (2018) established legal recognition of passive euthanasia and living wills.
UPSC Civil Services Examination, Previous Year Questions (PYQs)
Prelims
Q. Right to Privacy is protected as an intrinsic part of Right to Life and Personal Liberty. Which of the following in the Constitution of India correctly and appropriately imply the above statement? (2018)
(a) Article 14 and the provisions under the 42nd Amendment to the Constitution.
(b) Article 17 and the Directive Principles of State Policy in Part IV.
(c) Article 21 and the freedoms guaranteed in Part III.
(d) Article 24 and the provisions under the 44th Amendment to the Constitution.
Ans: (C)
Mains
Q. In order to enhance the prospects of social development, sound and adequate health care policies are needed particularly in the fields of geriatric and maternal health care.Discuss.(2020)