Passive Euthanasia and the Right to Die with Dignity | 28 Nov 2025
Why in News?
The Supreme Court has instructed a hospital to constitute a medical board to assess a petition seeking passive euthanasia for a 32-year-old individual who has remained in a “persistent vegetative state” for the past 12 years.
- A Persistent Vegetative State (PVS) is a medical condition in which a person loses higher brain functions (like awareness, thinking, and purposeful movement) but retains basic bodily functions such as breathing, circulation, sleep–wake cycles, and reflexes.
What is Euthanasia?
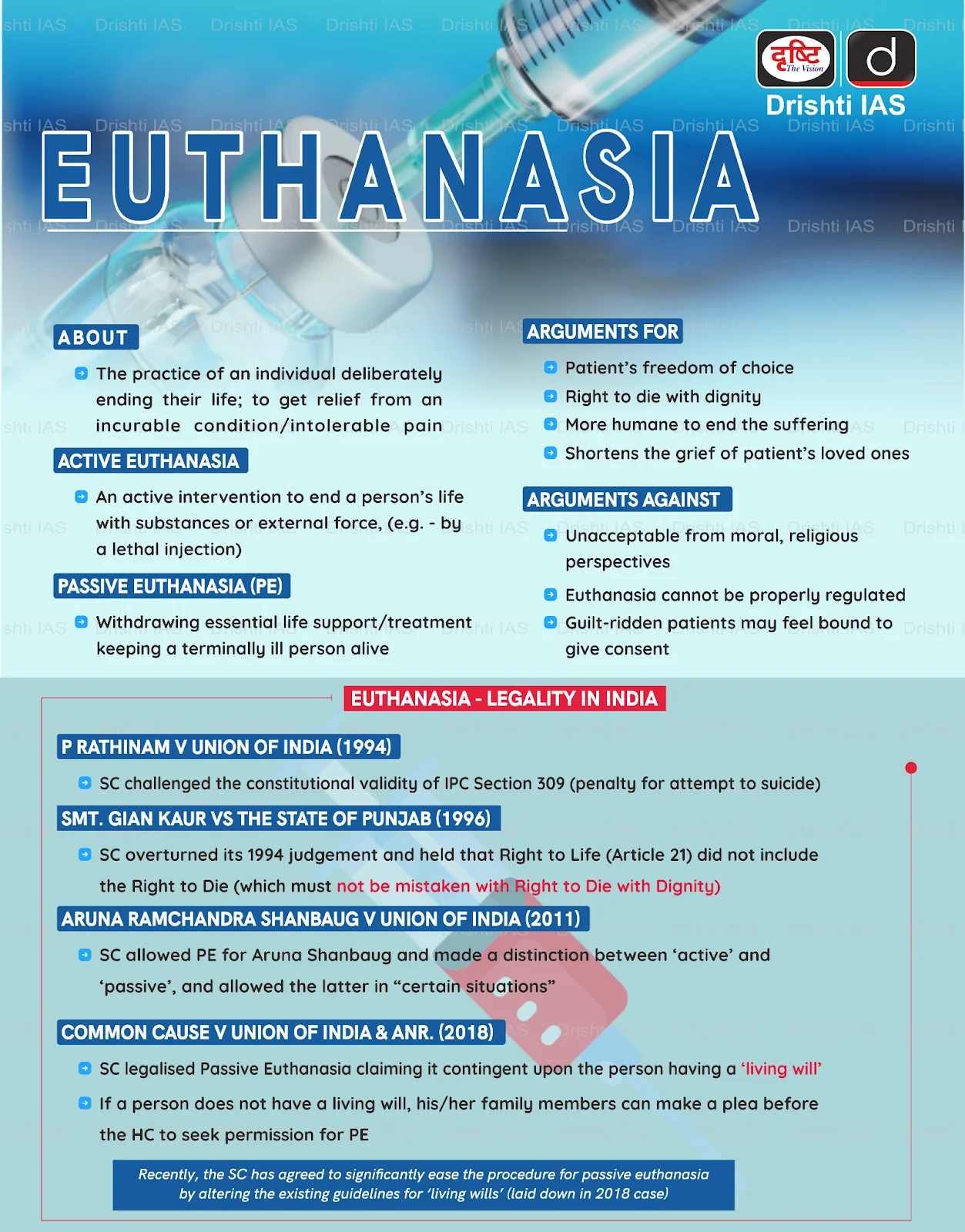
- About: Euthanasia refers to intentionally accelerating a person’s death to prevent further suffering from an incurable or terminal illness. It involves a painless, deliberate act aimed at relieving physical, emotional, or spiritual distress. It is of two types:
- Active Euthanasia: It involves deliberately ending a patient’s life. It can take different forms:
- Voluntary, where the patient consciously opts for death;
- Non-voluntary, where the decision is made for an incompetent patient; and
- Involuntary, where death is caused without consent (almost illegal in all countries).
- Passive Euthanasia: It allows a terminally ill patient to die naturally by withdrawing or withholding life-sustaining treatment.
- This approach aims to uphold the right to die with dignity and prevent prolonged, futile suffering in irreversible medical conditions.
- Active Euthanasia: It involves deliberately ending a patient’s life. It can take different forms:
- Legal Standing in India:
- Active Euthanasia: Indian law prohibits active euthanasia. The Bharatiya Nyaya Sanhita (BNS), 2023, categorizes any deliberate act causing death as an offense, prosecutable under its sections on culpable homicide (Section 100) or murder (Section 101).
- Passive Euthanasia: The Supreme Court (SC) has recognised passive euthanasia under certain restrictions, as long as it is in the best interests of the patient and follows the law.
- Article 21 guarantees that no one shall be deprived of life or personal liberty except by law, and the Supreme Court interprets it to include health, livelihood, privacy, shelter, and dignity, but it does not include the right to die, except under certain circumstances allowing a dignified death
- Law Commission Stand: The 241st Report of the Law Commission (2012) clarified that a competent patient can refuse life-sustaining treatment without legal consequences, and doctors acting according to the patient’s informed wishes are not guilty of abetment or culpable homicide.
- Related Judicial Pronouncements:
- Maruti Shripati Dubal v. State of Maharashtra (1987): The Bombay High Court held that the right to die forms part of the right to life under Article 21, and that individuals who are terminally ill or experiencing severe pain should be allowed to choose to end their lives.
- Gian Kaur v. State of Punjab (1996): The SC stated that the right to life does not include the right to die, emphasizing that life is a natural gift that should be preserved rather than terminated.
- Aruna Shanbaug v. Union of India (2011): The SC allowed withholding or withdrawing life-sustaining treatment, even for patients who cannot make decisions but only under strict legal and medical safeguards.
- Common Cause v. Union of India (2018): The SC noted that active euthanasia (deliberate action to cause death) and passive euthanasia (withdrawing life-saving treatment) are distinct, stating that passive euthanasia may be permitted in rare cases.
- The Court established that a terminally ill patient has a fundamental right to die with dignity, which includes the right to refuse medical treatment through advance medical directives, known as living wills.
- Supreme Court Directives on Euthanasia:
- Original 2018 Directives: The 2018 guidelines required a two-stage medical review:
- Primary Medical Board: Constituted by the hospital, including the Head of the treating department and at least 3 specialists from general medicine, cardiology, neurology, nephrology, psychiatry, or oncology, each with 20 years of experience.
- Secondary Medical Board: Appointed by the district collector, including the Chief District Medical Officer as Chairman and three expert doctors from the same fields.
- 2023 Modifications: The Supreme Court retained both boards but reduced the experience requirement from 20 years to five and set a 48-hour time limit for opinions.
- The secondary board now excludes the Chief District Medical Officer, allows a nominee by the District Medical Officer, and both boards have three members each.
- Original 2018 Directives: The 2018 guidelines required a two-stage medical review:
- Global Position on Euthanasia: Netherlands, Luxembourg, and Belgium allow both euthanasia and assisted suicide for anyone experiencing unbearable suffering with no chance of improvement.
- Switzerland permits non-physicians to help the terminally ill commit suicide, though active euthanasia is illegal.
- Australia also allows both types, limited to adults with full decision-making capacity who have a terminal illness.
- These global variations highlight how euthanasia remains ultimately an ethical question, shaped less by medical capacity and more by each society’s moral principles, values, and philosophical traditions.
What are the Key Ethical Perspectives on Euthanasia?
|
Arguments FOR Euthanasia (Pro-Choice) |
Arguments AGAINST Euthanasia (Pro-Life) |
|
Supremacy of Autonomy (Libertarianism): Drawing from John Stuart Mill’s Liberalism, proponents argue that an individual is sovereign over their own body and mind. Therefore, a competent adult has the libertarian right to self-determination, including the choice to end their life when it becomes unbearable, without state interference. |
The Sanctity of Life (Deontology): Immanuel Kant’s Deontological ethics asserts that human life is an "end in itself" and never a means to an end. Therefore, intentionally destroying life—even to escape pain—treats humanity merely as a tool, violating the Natural Law duty to preserve life regardless of its quality. |
|
Minimizing Suffering (Utilitarianism): Based on Jeremy Bentham’s Act Utilitarianism, the moral worth of an action is determined by its ability to maximize happiness and minimize pain. Since prolonged agony serves no purpose, euthanasia is viewed as a compassionate, rational choice that reduces the net suffering in the world. |
Value of Endurance (Virtue Ethics): Virtue Ethicists argue that suffering, while painful, is a part of the human condition that calls for the virtues of courage and endurance. Gandhian ethics (Ahimsa) generally rejects active killing, suggesting that spiritual strength is found in facing life's natural end rather than prematurely escaping it. |
|
Beneficence Over Biology: The medical principle of Beneficence (acting in the patient's best interest) implies that a doctor's duty is to relieve suffering. When a cure is impossible and pain is unmanageable, aiding a peaceful death is seen as fulfilling the humanitarian obligation of the medical profession. |
"Do No Harm" (Non-Maleficence): The core of medical ethics, rooted in the Hippocratic Oath, is Primum non nocere (First, do no harm). Opponents argue that a doctor is a healer, not an executioner; engaging in euthanasia corrupts the telos (purpose) of medicine and destroys the doctor-patient trust. |
|
Rational Resource Management (Pragmatism): From a pragmatic utilitarian standpoint, maintaining life support for PVS (Persistent Vegetative State) patients consumes scarce medical resources. Redirecting these funds to treatable patients upholds the principle of Distributive Justice, ensuring the greatest good for the greatest number. |
The "Slippery Slope" (Rule Utilitarianism): Rule Utilitarians warn that even if a specific case of euthanasia seems merciful, legalizing it creates a dangerous rule. It risks a "Slippery Slope" where society eventually starts justifying the involuntary killing of the elderly, disabled, or poor to save costs, leading to moral decay. |
Did you Know?
- Euthanasia and assisted suicide are different: euthanasia involves someone, usually a doctor, directly ending a patient’s life, while assisted suicide provides the means or guidance for a person to end their own life.
- Suicide tourism, or euthanasia tourism, occurs when patients travel to countries where these practices are legal. Switzerland is a major destination, attracting patients mainly from the UK, Germany, and France.
Conclusion
The Supreme Court’s intervention reinforces India’s evolving approach to the right to die with dignity, combining legal safeguards with compassionate care through a structured, medically-reviewed passive euthanasia process.
|
Drishti Mains Question: Differentiate between active and passive euthanasia. What are the procedural safeguards mandated by the Supreme Court for the withdrawal of life support? |
Frequently Asked Questions (FAQs)
Q. What is the key difference between active and passive euthanasia?
Active euthanasia involves a direct act to end a life (e.g., lethal injection), while passive euthanasia is the withdrawal of life-sustaining treatment to allow a natural death from the underlying illness.
Q. Which landmark Supreme Court judgment recognized the 'Right to Die with Dignity' as part of Article 21?
The Common Cause v. Union of India (2018) judgment recognized this right and legally permitted passive euthanasia and 'living wills' in India.
Q. How did the Supreme Court recognize passive euthanasia in India?
In Aruna Shanbaug v. Union of India (2011) and Common Cause v. Union of India (2018), the SC legalized passive euthanasia and advance medical directives under Article 21.
UPSC Civil Services Examination, Previous Year Questions (PYQs)
Prelims
Q. Right to Privacy is protected as an intrinsic part of Right to Life and Personal Liberty. Which of the following in the Constitution of India correctly and appropriately imply the above statement? (2018)
(a) Article 14 and the provisions under the 42nd Amendment to the Constitution.
(b) Article 17 and the Directive Principles of State Policy in Part IV.
(c) Article 21 and the freedoms guaranteed in Part III.
(d) Article 24 and the provisions under the 44th Amendment to the Constitution.
Ans: (c)
Mains
Q. In order to enhance the prospects of social development, sound and adequate health care policies are needed particularly in the fields of geriatric and maternal health care.Discuss. (2020)