Euthanasia Debate in India | 19 Jan 2026
For Prelims: Bharatiya Nyaya Sanhita (BNS), 2023, Supreme Court, Article 21, Law Commission, High Court, Ayushman Bharat, ASHA.
For Mains: Overview of euthanasia, covering its key definitions, the principal arguments for and against its legalization, and potential pathways forward.
Why in News?
The Supreme Court is hearing Harish Rana vs Union of India (2025), a plea seeking permission for passive euthanasia through withdrawal of life-sustaining treatment.
- The petitioner has been bedridden for over 13 years with 100% quadriplegic disability after sustaining severe head injuries from a fourth-floor fall.
Summary
- The Supreme Court has reserved its judgment in Harish Rana vs Union of India (2025), a crucial case seeking permission for passive euthanasia.
- Active euthanasia is illegal, but the Supreme Court has legalized passive euthanasia (withdrawing treatment) under strict guidelines to uphold the 'right to die with dignity' under Article 21.
- The case reignites the ethical conflict between upholding individual autonomy for a dignified death and preventing potential misuse against vulnerable populations.
What is Euthanasia?
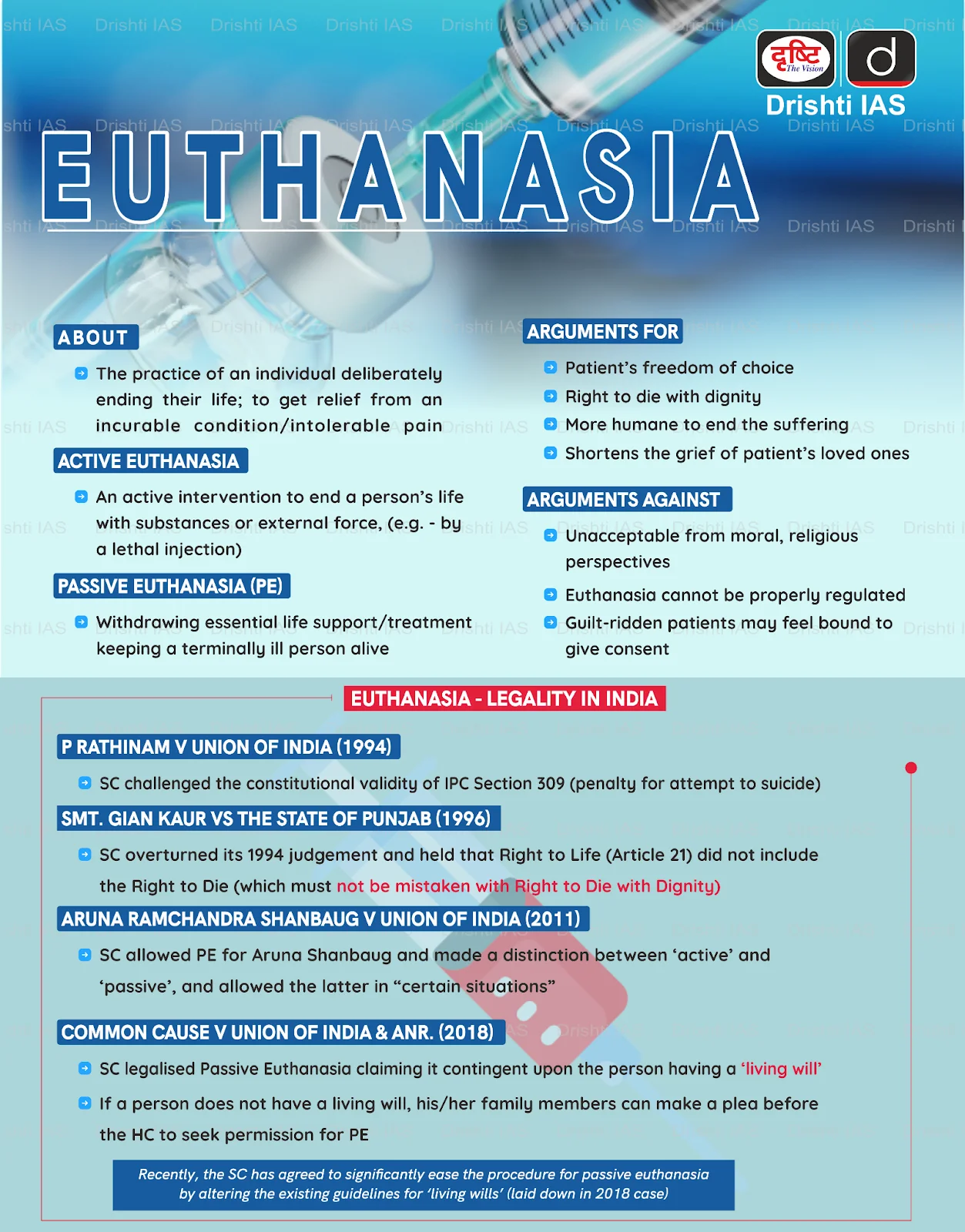
- About: Euthanasia refers to the intentional hastening of death to relieve unbearable suffering caused by an incurable or terminal illness. It aims to reduce physical pain, emotional distress, and spiritual suffering through a deliberate and painless intervention.
- The debate around euthanasia is not merely medical; it is deeply rooted in ethical values, human rights, and societal beliefs.
- Forms and Classifications of Euthanasia: It is primarily categorized into Active Euthanasia (a deliberate act like lethal injection) and Passive Euthanasia (withholding or withdrawing life-sustaining treatment).
- These are further divided into Voluntary (patient-consented), Non-voluntary (decision for an incompetent patient), and Involuntary (without consent, widely illegal) forms.
- Legal Framework in India:
- Indian law explicitly prohibits active euthanasia. The Bharatiya Nyaya Sanhita (BNS), 2023, treats any intentional causing of death as an offence under Section 100 (culpable homicide) or Section 101 (murder).
- The Supreme Court (SC) has legalized passive euthanasia under a strict regulatory framework, recognizing the right to die with dignity as part of Article 21 (Right to Life).
- The Law Commission's 241st Report (2012) clarified that a competent patient’s refusal of life-sustaining treatment is legally valid and doctors following such informed wishes cannot be charged with abetment or culpable homicide.
- Judgements Related to Euthanasia in India:
- Maruti Shripati Dubal v. State of Maharashtra (1987): The Bombay High Court held that the right to die is part of Article 21 (Right to Life), allowing terminally ill persons or those in severe pain to end their lives.
- Gian Kaur v. State of Punjab (1996): The SC reversed this view, holding that the right to life does not include the right to die, and emphasized preservation of life.
- Aruna Shanbaug v. Union of India (2011): The SC permitted passive euthanasia (withholding or withdrawing life support) under strict legal and medical safeguards, even for patients unable to consent.
- Common Cause v. Union of India (2018): The SC distinguished active euthanasia (not permitted) from passive euthanasia (permitted in rare cases) and recognized the right to die with dignity, including refusal of treatment through living wills (advance medical directives).
- Procedure for Passive Euthanasia in India:
- The SC 2018 directives mandated a two-stage medical review by a Primary and a Secondary Medical Board.
- Primary Medical Board: Formed by the hospital, comprising the Head of the treating department and at least three senior specialists from fields such as general medicine, cardiology, neurology, nephrology, psychiatry, or oncology, each with 20 years’ experience.
- Secondary Medical Board: Constituted by the District Collector, headed by the Chief District Medical Officer, along with three expert doctors from the same medical specialties.
- In 2023, the Supreme Court simplified the process by keeping both boards but reducing the required specialist experience from 20 years to 5 and setting a strict 48-hour deadline for their opinions.
- The Secondary Board was also modified, replacing the Chief District Medical Officer as chairman with a nominee from the District Medical Officer, and both boards now consist of three members each.
- The SC 2018 directives mandated a two-stage medical review by a Primary and a Secondary Medical Board.
- Global Legal Landscape on Euthanasia: The Netherlands, Belgium, Luxembourg, Spain, Quebec (Canada), and parts of Australia permit both euthanasia and physician-assisted suicide under strict conditions.
- Switzerland allows assisted suicide by non-physicians but prohibits active euthanasia.
- Sweden and France permit passive euthanasia, while Italy recognizes the right to refuse treatment.
- Ethical and Practical Controversies: The euthanasia debate is fundamentally polarized between arguments for personal autonomy and a "death with dignity" and opposing arguments grounded in the sanctity of life and the "do no harm" principle of the Hippocratic Oath.
- It is further complicated by practical concerns over accurately assessing a patient's mental competency and the ethical risks of potential misuse or a slippery slope in medical judgment.
What are the Key Arguments in Favor of Legalizing Euthanasia?
- Upholding Individual Autonomy: Central to the argument is the principle of patient autonomy and self-determination, which the Supreme Court upheld in Common Cause vs Union of India (2018) by recognizing the "right to die with dignity" under Article 21 and legalizing advanced medical directives.
- Alleviating Incurable Suffering: Euthanasia is advocated to relieve unbearable suffering in terminal illnesses, a position supported by data from permissive countries where its use is predominantly for severe conditions like advanced cancer.
- Curbing Futile Medical Intervention: It prevents futile, suffering-prolonging treatment, alleviating emotional and financial burdens on families and healthcare systems, as exemplified by the passive euthanasia permitted in India since the Aruna Shanbaug case (2011) for withdrawing non-beneficial interventions.
- Philosophical and Pragmatic Foundations: Libertarian principles (John Stuart Mill) defend the right to choose euthanasia based on bodily autonomy, while utilitarian ethics (Jeremy Bentham) support it to minimize suffering. This aligns with the medical duty to relieve pain and allows for a just allocation of healthcare resources.
What are the Principal Arguments Against the Legalization of Euthanasia?
- Ethical and Moral Conflict: Many view euthanasia as violating the sanctity of life, a stance rooted in religious, cultural, and deontological ethics (Immanuel Kant) that sees life as an inviolable end in itself.
- High Risk of Abuse and Coercion: Vulnerable populations, the elderly, disabled, and financially dependent, are at significant risk of being pressured into euthanasia, especially in a country with socioeconomic disparities and uneven healthcare access.
- Challenges in Assessing True Consent: Many Indian psychiatrists lack confidence in detecting depression or subtle coercion in terminally ill patients, raising the risk of inappropriate approvals.
- Stringent Legal Prohibitions and Ambiguity: The BNS, 2023, prosecutes such acts under Sections 100 (culpable homicide), 101 (murder), and 108 (abetment of suicide), creating legal peril for practitioners in the absence of clear regulatory legislation.
- Cumbersome and Inaccessible Procedures: Passive euthanasia, under the SC guidelines, involves a slow, court-driven process with multiple medical boards, making it inaccessible for many and increasing the judicial burden.
How can India Strengthen its End-of-life Care Framework?
- Legislative Clarity: Enact a clear parliamentary law codifying the SC's 2018 guidelines on passive euthanasia and Advance Medical Directives (Living Wills), providing legal protection for practitioners.
- Procedural Streamlining: Simplify processes by decentralizing oversight to district-level committees or multidisciplinary hospital ethics committees, and integrate living wills into the National Health Digital Record for easy access, as initiated by the Supreme Court's 2023 simplification.
- Universal Palliative Care Access: Prioritize and institutionalize hospice and palliative care by establishing a network of home-based, community-led, and hospital-based services, leveraging Ayushman Bharat for coverage and training ASHA workers in basic pain management.
- Rigorous Safeguards: Implement mandatory independent psychiatric evaluations, social worker assessments, and cooling-off periods to screen for coercion of vulnerable groups (elderly, disabled) and ensure genuine patient autonomy.
- Public Awareness and Consensus: Launch nationwide campaigns to educate the public and professionals about living wills and end-of-life choices, while fostering public dialogue involving medical bodies, legal experts, ethicists, and religious leaders to build an ethical consensus.
Conclusion
The Harish Rana case highlights the urgent need for a clear legislative framework on passive euthanasia and advanced medical directives. While patient autonomy and relief from suffering are compelling, the risk of misuse, coercion, and legal ambiguity demands strong safeguards, palliative care expansion, and procedural streamlining to protect vulnerable citizens.
|
Drishti Mains Question: The right to die with dignity is an extension of the right to live with dignity. Critically analyze this statement in the context of the judicial evolution of euthanasia jurisprudence in India. |
Frequently Asked Questions (FAQs)
1. What is passive euthanasia in India?
Passive euthanasia involves withdrawing or withholding life-sustaining treatment, permitted under strict safeguards by the Supreme Court since Aruna Shanbaug (2011) and Common Cause (2018).
2. Is active euthanasia legal in India?
No. Active euthanasia is illegal and treated as culpable homicide or murder under BNS 2023 Sections 100 and 101, with abetment of suicide under Section 108.
3. What is an advance medical directive (living will)?
It is a legal document allowing a competent adult to refuse life-sustaining treatment in advance, recognised by the Supreme Court in Common Cause (2018).
UPSC Civil Services Examination, Previous Year Questions (PYQs)
Prelims
Q. Right to Privacy is protected as an intrinsic part of Right to Life and Personal Liberty. Which of the following in the Constitution of India correctly and appropriately imply the above statement? (2018)
(a) Article 14 and the provisions under the 42nd Amendment to the Constitution.
(b) Article 17 and the Directive Principles of State Policy in Part IV.
(c) Article 21 and the freedoms guaranteed in Part III.
(d) Article 24 and the provisions under the 44th Amendment to the Constitution.
Ans: (c)
Mains
Q. In order to enhance the prospects of social development, sound and adequate health care policies are needed particularly in the fields of geriatric and maternal health care.Discuss. (2020)